Volume 8, Issue 2 (Journal of Clinical and Basic Research (JCBR) 2024)
jcbr 2024, 8(2): 1-4 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abdulraheem Handhal A, Gholipur M, Mohammad zadeh F, Ghorbani S, Khajeniazi S. Evaluation of the relationship between Hs-CRP and lipid profile in patients with hypothyroidism. jcbr 2024; 8 (2) :1-4
URL: http://jcbr.goums.ac.ir/article-1-444-en.html
URL: http://jcbr.goums.ac.ir/article-1-444-en.html
Ameer Abdulraheem Handhal1 

 , Mahin Gholipur2
, Mahin Gholipur2 

 , Fatima Mohammad zadeh2
, Fatima Mohammad zadeh2 

 , Somayeh Ghorbani3
, Somayeh Ghorbani3 

 , Safoura Khajeniazi *4
, Safoura Khajeniazi *4 




 , Mahin Gholipur2
, Mahin Gholipur2 

 , Fatima Mohammad zadeh2
, Fatima Mohammad zadeh2 

 , Somayeh Ghorbani3
, Somayeh Ghorbani3 

 , Safoura Khajeniazi *4
, Safoura Khajeniazi *4 


1- Department of Clinical Biochemistry, School of Medical Sciences, Golestan University of Medical Sciences, Gorgan,Iran
2- Metabolic Disorders Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Cancer Research Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Clinical Biochemistry, School of Medical Sciences, Golestan University of Medical Sciences, Gorgan,Iran; Metabolic Disorders Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,niazie80@gmail.com
2- Metabolic Disorders Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Cancer Research Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Clinical Biochemistry, School of Medical Sciences, Golestan University of Medical Sciences, Gorgan,Iran; Metabolic Disorders Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,
Full-Text [PDF 443 kb]
(692 Downloads)
| Abstract (HTML) (1654 Views)
Full-Text: (318 Views)
Introduction
Hypothyroidism, a prevalent condition characterized by thyroid dysfunction, often presents with elevated serum thyroid-stimulating hormone (TSH) levels and normal free thyroxine (fT4) levels (1-3). Thyroid hormones exert significant influence on various metabolic pathways, regulating a broad spectrum of metabolic parameters. The thyroid gland notably acts as an effector of lipoprotein metabolism, which encompasses several cardiovascular disease (CVD) risk factors. Consequently, thyroid function can impact overall CVD risk. A linear increase in total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TGs) has been observed even within the normal TSH range. Conversely, a linear decrease in high-density lipoprotein cholesterol (HDL-C) has been noted with increasing TSH levels (4-6). Hypothyroidism is a major cause of secondary dyslipidemia due to the crucial role thyroid hormones play in lipid synthesis (7). Several studies have established a link between subclinical hypothyroidism (SCH) and obesity, dyslipidemia, and metabolic syndrome (8-11).
C-reactive protein (CRP), an acute-phase inflammatory protein activated during inflammatory conditions, serves as a clinical marker for detecting inflammation, infection, and tissue damage (12). Additionally, it has been suggested that CRP levels may be used to assess arterial rigidity and its improvement in hypothyroid patients. However, CRP measurement is not routinely employed for diagnosing thyroid diseases (13). Previous studies have demonstrated the ability of progressive hypothyroid failure to elevate CRP levels, potentially representing an additional risk factor for developing cardiovascular diseases in individuals with hypothyroidism (14). Recent research has highlighted high-sensitivity C-reactive protein (Hs-CRP) as a stronger predictor of CVD among numerous inflammatory markers, even surpassing low-density lipoprotein cholesterol (LDL-C) (15,16). However, conflicting results exist regarding the role of Hs-CRP as a shared risk factor for SCH and coronary artery diseases (17-20).
The present study aimed to evaluate serum Hs-CRP levels, lipid profiles, and their relationship with thyroid hormones in patients with hypothyroidism compared to a control group.
Methods
Sample Collection
This case-control study involved 45 hypothyroid patients and 45 healthy controls recruited at Deziani Hospital in Gorgan, Iran, between November 2022 and February 2023. Data were recorded directly to facilitate study management.
All participants meeting the inclusion criteria provided informed consent. Case and control groups were matched for age and sex. Five milliliters of blood were drawn from each participant without anticoagulant, followed by immediate centrifugation to obtain serum for biomarker analysis.
Inclusion criteria
Hypothyroidism, a prevalent condition characterized by thyroid dysfunction, often presents with elevated serum thyroid-stimulating hormone (TSH) levels and normal free thyroxine (fT4) levels (1-3). Thyroid hormones exert significant influence on various metabolic pathways, regulating a broad spectrum of metabolic parameters. The thyroid gland notably acts as an effector of lipoprotein metabolism, which encompasses several cardiovascular disease (CVD) risk factors. Consequently, thyroid function can impact overall CVD risk. A linear increase in total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TGs) has been observed even within the normal TSH range. Conversely, a linear decrease in high-density lipoprotein cholesterol (HDL-C) has been noted with increasing TSH levels (4-6). Hypothyroidism is a major cause of secondary dyslipidemia due to the crucial role thyroid hormones play in lipid synthesis (7). Several studies have established a link between subclinical hypothyroidism (SCH) and obesity, dyslipidemia, and metabolic syndrome (8-11).
C-reactive protein (CRP), an acute-phase inflammatory protein activated during inflammatory conditions, serves as a clinical marker for detecting inflammation, infection, and tissue damage (12). Additionally, it has been suggested that CRP levels may be used to assess arterial rigidity and its improvement in hypothyroid patients. However, CRP measurement is not routinely employed for diagnosing thyroid diseases (13). Previous studies have demonstrated the ability of progressive hypothyroid failure to elevate CRP levels, potentially representing an additional risk factor for developing cardiovascular diseases in individuals with hypothyroidism (14). Recent research has highlighted high-sensitivity C-reactive protein (Hs-CRP) as a stronger predictor of CVD among numerous inflammatory markers, even surpassing low-density lipoprotein cholesterol (LDL-C) (15,16). However, conflicting results exist regarding the role of Hs-CRP as a shared risk factor for SCH and coronary artery diseases (17-20).
The present study aimed to evaluate serum Hs-CRP levels, lipid profiles, and their relationship with thyroid hormones in patients with hypothyroidism compared to a control group.
Methods
Sample Collection
This case-control study involved 45 hypothyroid patients and 45 healthy controls recruited at Deziani Hospital in Gorgan, Iran, between November 2022 and February 2023. Data were recorded directly to facilitate study management.
All participants meeting the inclusion criteria provided informed consent. Case and control groups were matched for age and sex. Five milliliters of blood were drawn from each participant without anticoagulant, followed by immediate centrifugation to obtain serum for biomarker analysis.
Inclusion criteria
- All participants (both hypothyroid patients and controls) were over 18 years old.
- All patients had hypothyroidism.
- All patients were newly diagnosed (untreated hypothyroidism).
Exclusion criteria
- Pregnant and lactating women.
- Patients with autoimmune diseases.
- Patients taking steroid supplements.
- Patients with inherited thyroid disease.
- Patients with chronic conditions like diabetes mellitus and heart disease.
Experiments
Following sample collection, tubes were centrifuged to separate serum, which was subsequently used for biochemical marker analysis. All markers were measured using commercial kits. ELISA assayed T3, T4, and TSH, while TG, HDL, LDL, VLDL, and total cholesterol were measured by spectroscopy using a Mindray BS-380 automated analyzer (China). Serum Hs-CRP levels were determined using a commercial ELISA kit at a private laboratory, following the manufacturer's instructions.
Chemicals
Kits for determining TSH, T3, and T4 were obtained from Pishtaz Teb Diagnostics. Kits for TG, HDL, LDL, VLDL, and total cholesterol measurement were procured from Pars Azmoon. Hs-CRP levels were quantified using a kit from ZellBio GmbH.
Statistical Analysis
Data analysis was performed using SPSS software (version 18). The Shapiro-Wilk test was employed to assess data normality. Spearman correlation and the Mann-Whitney U test were utilized to evaluate correlations and compare serum Hs-CRP levels and other parameters between groups. Continuous variables are presented as median (interquartile range), and statistical significance is indicated by a P-value < 0.05.
Results
The research involved a total of 90 participants, consisting of 45 patients with hypothyroidism (14 males and 31 females), and 45 individuals without the condition (11 males and 34 females). The results showed a significant difference in the level of thyroid hormone panel between the hypothyroid patients and healthy subjects. The level of TSH in hypothyroid subjects was significantly higher, and T3 and T4 levels were lower than their levels in normal individuals (P-value < 0.05).
According to Table 1, the level of Hs-CRP in hypothyroid patients was higher than that in normal individuals, but this difference was not significant (P-value = 0.09). Also, the components of the lipid profile, including CHO, VLDL, LDL, and HDL in the case, were higher than those in control insignificantly (P-value > 0.05). Measurement of TG level in the control group showed this parameter was higher than in subjects suffering hypothyroidism P-value = 0.9.
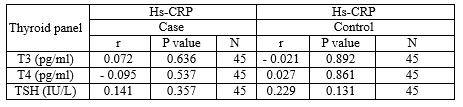
According to the Table 2, Hs-CRP, it has a positive correlation with TSH T3 and a negative correlation with T4 in subjects with hypothyroidism. All of the correlations were not significant < 0.05).
Table 3 shows a positive correlation between Hs-CRP and all lipid profile components except HDL. There was a negative correlation between Hs-CRP and HDL. Also, Hs-CRP has a negative correlation with T3. In addition, the correlation of Hs-CRP and TG and VLDL in healthy subjects is significant.
Table 4 shows a correlation between thyroid hormone levels and lipid profile in hypothyroidism patients. Statistical evaluation of the result demonstrates the positive correlation between TG, CHO, VLDL, and LDL with T3 and T4, but HDL has a negative correlation with them. In addition, TG, CHO, VLDL, and LDL, with the exception of HDL, have a negative correlation with TSH. The correlation between TG and VLDL with T3 and T4 is significant, and the correlation between other parameters is insignificant.
Discussion
This study investigated serum Hs-CRP levels, lipid profiles, and their relationship with thyroid hormones in patients with hypothyroidism compared to a control group. The findings revealed significantly higher TSH levels in hypothyroid subjects compared to controls. While Hs-CRP levels were also higher in hypothyroid patients, this difference did not reach statistical significance.
In contrast to the findings, Jose et al. (2016) found no association between TSH and Hs-CRP in subclinical hypothyroidism (1). The data, however, indicate a positive correlation between Hs-CRP and TSH in hypothyroid patients, aligning with the observations of Shantha et al. (2008), who suggested a potential link between systemic inflammation and subclinical hypothyroidism (20). This is further supported by Czarnywojtek et al. (2014), who investigated the utility of high-sensitivity CRP (Hs-CRP) measurement in distinguishing types of amiodarone-induced thyrotoxicosis (AIT). While they found no significant difference in Hs-CRP levels between AIT types I and II, they did observe a significant negative correlation between Hs-CRP and TSH, a finding that contrasts with the non-significant positive correlation observed in both patient and control groups in the study (13).
Krishnamurthy et al. (2022) investigated the role of chronic inflammation in the progression from subclinical hypothyroidism (SCH) to overt hypothyroidism, along with the relationship between hypothyroidism, lipid abnormalities, and cardiac dysfunction. They found that chronic inflammation, assessed by Hs-CRP levels, is a significant risk factor for this progression and is often associated with dyslipidemia (21). Similarly, Ahmad et al. (2018) demonstrated a significant positive correlation between TSH and Hs-CRP in thyroid disorders (22). Sharma et al. also reported elevated Hs-CRP levels in thyroid disorders, with significantly higher levels observed in hypothyroid patients compared to hyperthyroid patients (23).
Further supporting a link between hypothyroidism and cardiovascular disease, Ahmad et al. (2022) showed that Hs-CRP levels were significantly elevated in hypothyroid patients compared to controls and correlated significantly with cardiovascular risk factors, including total cholesterol and high-density lipoprotein (HDL) cholesterol (24). Ganesan et al. (2021) focused on the relationship between Hs-CRP and TSH in subclinical hypothyroidism, finding a significant positive correlation between the two. Their study also noted higher levels of inflammatory markers and lipid profiles in patients with SCH compared to euthyroid individuals, though no correlation was found between Hs-CRP, TSH, and lipid profile. This observation aligns with the study, which also demonstrated a positive, albeit non-significant, correlation between Hs-CRP and TSH (15).
Sharma et al. (2016) specifically evaluated lipid profiles and Hs-CRP levels in patients with SCH, revealing a significant positive correlation between TSH levels and lipids (total cholesterol, LDL-C, triglycerides, and VLDL-C) and Hs-CRP.
In their 2016 study, Sharma et al. found a significant positive correlation between TSH levels and various lipids (total cholesterol, LDL-C, triglycerides, and VLDL-C) in individuals with subclinical hypothyroidism (SCH). Conversely, HDL-C exhibited a non-significant inverse correlation with TSH. Furthermore, a significant positive correlation was observed between TSH and Hs-CRP levels in SCH patients compared to controls (17).
Kshetrimayum et al. (2019) investigated Hs-CRP levels and lipid profiles in adults with hypothyroidism at a tertiary care hospital. They compared thyroid hormone profiles, Hs-CRP, and lipid profiles in newly diagnosed hypothyroid adults to controls and also compared these parameters between subclinical and clinical hypothyroid patients. Notably, they found that dyslipidemia, characterized by elevated total cholesterol and LDL-C, was a common finding in patients with clinical hypothyroidism (CH). Serum Hs-CRP levels were significantly elevated in hypothyroid cases but remained within the normal range in controls. Additionally, significant increases in LDL-C and TG, along with decreased HDL-C, were observed in hypothyroid patients, although the average serum cholesterol was lower in these individuals. The study also revealed a significant positive correlation between TSH and Hs-CRP in hypothyroid cases compared to controls (25,26).
Jublanc et al. (2004) assessed the relationship between circulating C-reactive protein (CRP) levels, thyroid hormone profiles, and cardiovascular risk in hyperlipidemic euthyroid individuals. They reported an association between low free thyroxine (FT4) levels and elevated Hs-CRP but no correlation between FT4 and CRP. This finding is partially consistent with the results, which showed a non-significant negative correlation between FT4 and CRP (27).
Rustam et al. (2021) evaluated osteopontin and Hs-CRP levels in Iraqi patients with hypothyroidism, finding elevated serum levels of Hs-CRP, total cholesterol, triglycerides, LDL-C, VLDL-C, and osteopontin compared to healthy controls. Additionally, they reported a positive correlation between Hs-CRP and both triglycerides and VLDL-C, contrasting with the results, which showed a non-significant positive correlation with TG and a negative correlation with VLDL-C (28).
Singh et al. (2021) analyzed lipid profiles, thyroid hormones, and Hs-CRP levels in newly diagnosed hypothyroid individuals and compared them to healthy controls, as well as between subclinical and clinical hypothyroid cases. They observed significantly higher Hs-CRP levels in cases and a significant positive correlation between TSH and Hs-CRP levels. Interestingly, they found lower levels of most lipid profile components in controls compared to cases, with the exception of HDL-C. Conversely, the study showed higher levels of most lipids in hypothyroid individuals, except for TG and total cholesterol.
Jha (2021) focused on thyroid hormone profiles, Hs-CRP, and lipid profiles in newly diagnosed hypothyroid adults, comparing them to healthy controls and between subclinical and clinical hypothyroidism. Hypertriglyceridemia and elevated Hs-CRP levels were more prevalent in clinical hypothyroidism compared to subclinical hypothyroidism. Additionally, serum triglyceride levels were significantly higher in hypothyroid cases compared to controls, and a significant positive correlation was observed between serum TSH and Hs-CRP levels in patients with clinical hypothyroidism (29).
Sumanth Kumar et al. (2020) investigated vitamin D, Hs-CRP, and lipid profiles in newly diagnosed hypothyroid patients. Their findings revealed a positive correlation between Hs-CRP and TSH and a significant negative correlation between HDL levels and TSH in hypothyroid patients (30). These results partially align with the observations, except for the HDL levels, which were higher in the hypothyroid patients and showed a non-significant positive correlation with TSH.
The statistical analysis demonstrated positive correlations between TG and VLDL with TSH, while HDL, LDL, and TG exhibited negative correlations with TSH. However, only the negative correlation between LDL and TSH was statistically significant. Additionally, negative correlations were observed between TG, total cholesterol, VLDL, and LDL (excluding HDL) with T3 and T4, though these correlations were not significant.
Conclusion
In this study, positive correlations were observed between Hs-CRP and TSH, T3, and TG, while negative correlations were noted with total cholesterol, VLDL-C, HDL-C, and T4 in hypothyroid subjects. The positive correlation between Hs-CRP and TSH, as well as TG and LDL-C, suggests a potential role for Hs-CRP as a mediator between thyroid disorders and cardiovascular disease. However, further research with larger sample sizes is needed to confirm these findings due to the lack of statistical significance in most of the results, potentially attributed to the smaller sample size compared to other studies.
Acknowledgement
The authors express their gratitude to Mrs. Nahid Poursharifi for her assistance in the experimental aspects of this study.
Funding sources
This project, registered with the Deputy of Research and Technology of Golestan University of Medical Sciences (Gorgan, Iran) under approval number 113232, was funded by Mr. Ameer Abdulraheem Handhal, an MSc student at Golestan University of Medical Sciences.
Ethical statement
Ethical approval for this study was obtained from Golestan University of Medical Sciences (Ethical number IR.GOUMS.REC.1401.565).
Conflicts of interest
The authors declare no conflicts of interest.
Author contributions
Ameer Abdulraheem Handhal: Wrote the proposal and conducted the experimental aspects of the study.
Mahin Gholipur: Collaborated in writing the proposal.
Fatima Mohammadzadeh: Collaborated in the sampling phase of the study.
Somayeh Ghorbani: Performed data analysis.
Safoura Khajeniazi: Supervised the thesis, interpreted results, and wrote the manuscript.
Following sample collection, tubes were centrifuged to separate serum, which was subsequently used for biochemical marker analysis. All markers were measured using commercial kits. ELISA assayed T3, T4, and TSH, while TG, HDL, LDL, VLDL, and total cholesterol were measured by spectroscopy using a Mindray BS-380 automated analyzer (China). Serum Hs-CRP levels were determined using a commercial ELISA kit at a private laboratory, following the manufacturer's instructions.
Chemicals
Kits for determining TSH, T3, and T4 were obtained from Pishtaz Teb Diagnostics. Kits for TG, HDL, LDL, VLDL, and total cholesterol measurement were procured from Pars Azmoon. Hs-CRP levels were quantified using a kit from ZellBio GmbH.
Statistical Analysis
Data analysis was performed using SPSS software (version 18). The Shapiro-Wilk test was employed to assess data normality. Spearman correlation and the Mann-Whitney U test were utilized to evaluate correlations and compare serum Hs-CRP levels and other parameters between groups. Continuous variables are presented as median (interquartile range), and statistical significance is indicated by a P-value < 0.05.
Results
The research involved a total of 90 participants, consisting of 45 patients with hypothyroidism (14 males and 31 females), and 45 individuals without the condition (11 males and 34 females). The results showed a significant difference in the level of thyroid hormone panel between the hypothyroid patients and healthy subjects. The level of TSH in hypothyroid subjects was significantly higher, and T3 and T4 levels were lower than their levels in normal individuals (P-value < 0.05).
According to Table 1, the level of Hs-CRP in hypothyroid patients was higher than that in normal individuals, but this difference was not significant (P-value = 0.09). Also, the components of the lipid profile, including CHO, VLDL, LDL, and HDL in the case, were higher than those in control insignificantly (P-value > 0.05). Measurement of TG level in the control group showed this parameter was higher than in subjects suffering hypothyroidism P-value = 0.9.
|
Table 2. Correlation between Hs-CRP and thyroid hormones and TSH in case and control
 |
|
Table 3. Correlation between Hs-CRP and thyroid hormones and TSH in case and control
.PNG) |
|
Table 4. Correlation between thyroid hormone level and lipid profile components in case
.PNG) |
Discussion
This study investigated serum Hs-CRP levels, lipid profiles, and their relationship with thyroid hormones in patients with hypothyroidism compared to a control group. The findings revealed significantly higher TSH levels in hypothyroid subjects compared to controls. While Hs-CRP levels were also higher in hypothyroid patients, this difference did not reach statistical significance.
In contrast to the findings, Jose et al. (2016) found no association between TSH and Hs-CRP in subclinical hypothyroidism (1). The data, however, indicate a positive correlation between Hs-CRP and TSH in hypothyroid patients, aligning with the observations of Shantha et al. (2008), who suggested a potential link between systemic inflammation and subclinical hypothyroidism (20). This is further supported by Czarnywojtek et al. (2014), who investigated the utility of high-sensitivity CRP (Hs-CRP) measurement in distinguishing types of amiodarone-induced thyrotoxicosis (AIT). While they found no significant difference in Hs-CRP levels between AIT types I and II, they did observe a significant negative correlation between Hs-CRP and TSH, a finding that contrasts with the non-significant positive correlation observed in both patient and control groups in the study (13).
Krishnamurthy et al. (2022) investigated the role of chronic inflammation in the progression from subclinical hypothyroidism (SCH) to overt hypothyroidism, along with the relationship between hypothyroidism, lipid abnormalities, and cardiac dysfunction. They found that chronic inflammation, assessed by Hs-CRP levels, is a significant risk factor for this progression and is often associated with dyslipidemia (21). Similarly, Ahmad et al. (2018) demonstrated a significant positive correlation between TSH and Hs-CRP in thyroid disorders (22). Sharma et al. also reported elevated Hs-CRP levels in thyroid disorders, with significantly higher levels observed in hypothyroid patients compared to hyperthyroid patients (23).
Further supporting a link between hypothyroidism and cardiovascular disease, Ahmad et al. (2022) showed that Hs-CRP levels were significantly elevated in hypothyroid patients compared to controls and correlated significantly with cardiovascular risk factors, including total cholesterol and high-density lipoprotein (HDL) cholesterol (24). Ganesan et al. (2021) focused on the relationship between Hs-CRP and TSH in subclinical hypothyroidism, finding a significant positive correlation between the two. Their study also noted higher levels of inflammatory markers and lipid profiles in patients with SCH compared to euthyroid individuals, though no correlation was found between Hs-CRP, TSH, and lipid profile. This observation aligns with the study, which also demonstrated a positive, albeit non-significant, correlation between Hs-CRP and TSH (15).
Sharma et al. (2016) specifically evaluated lipid profiles and Hs-CRP levels in patients with SCH, revealing a significant positive correlation between TSH levels and lipids (total cholesterol, LDL-C, triglycerides, and VLDL-C) and Hs-CRP.
In their 2016 study, Sharma et al. found a significant positive correlation between TSH levels and various lipids (total cholesterol, LDL-C, triglycerides, and VLDL-C) in individuals with subclinical hypothyroidism (SCH). Conversely, HDL-C exhibited a non-significant inverse correlation with TSH. Furthermore, a significant positive correlation was observed between TSH and Hs-CRP levels in SCH patients compared to controls (17).
Kshetrimayum et al. (2019) investigated Hs-CRP levels and lipid profiles in adults with hypothyroidism at a tertiary care hospital. They compared thyroid hormone profiles, Hs-CRP, and lipid profiles in newly diagnosed hypothyroid adults to controls and also compared these parameters between subclinical and clinical hypothyroid patients. Notably, they found that dyslipidemia, characterized by elevated total cholesterol and LDL-C, was a common finding in patients with clinical hypothyroidism (CH). Serum Hs-CRP levels were significantly elevated in hypothyroid cases but remained within the normal range in controls. Additionally, significant increases in LDL-C and TG, along with decreased HDL-C, were observed in hypothyroid patients, although the average serum cholesterol was lower in these individuals. The study also revealed a significant positive correlation between TSH and Hs-CRP in hypothyroid cases compared to controls (25,26).
Jublanc et al. (2004) assessed the relationship between circulating C-reactive protein (CRP) levels, thyroid hormone profiles, and cardiovascular risk in hyperlipidemic euthyroid individuals. They reported an association between low free thyroxine (FT4) levels and elevated Hs-CRP but no correlation between FT4 and CRP. This finding is partially consistent with the results, which showed a non-significant negative correlation between FT4 and CRP (27).
Rustam et al. (2021) evaluated osteopontin and Hs-CRP levels in Iraqi patients with hypothyroidism, finding elevated serum levels of Hs-CRP, total cholesterol, triglycerides, LDL-C, VLDL-C, and osteopontin compared to healthy controls. Additionally, they reported a positive correlation between Hs-CRP and both triglycerides and VLDL-C, contrasting with the results, which showed a non-significant positive correlation with TG and a negative correlation with VLDL-C (28).
Singh et al. (2021) analyzed lipid profiles, thyroid hormones, and Hs-CRP levels in newly diagnosed hypothyroid individuals and compared them to healthy controls, as well as between subclinical and clinical hypothyroid cases. They observed significantly higher Hs-CRP levels in cases and a significant positive correlation between TSH and Hs-CRP levels. Interestingly, they found lower levels of most lipid profile components in controls compared to cases, with the exception of HDL-C. Conversely, the study showed higher levels of most lipids in hypothyroid individuals, except for TG and total cholesterol.
Jha (2021) focused on thyroid hormone profiles, Hs-CRP, and lipid profiles in newly diagnosed hypothyroid adults, comparing them to healthy controls and between subclinical and clinical hypothyroidism. Hypertriglyceridemia and elevated Hs-CRP levels were more prevalent in clinical hypothyroidism compared to subclinical hypothyroidism. Additionally, serum triglyceride levels were significantly higher in hypothyroid cases compared to controls, and a significant positive correlation was observed between serum TSH and Hs-CRP levels in patients with clinical hypothyroidism (29).
Sumanth Kumar et al. (2020) investigated vitamin D, Hs-CRP, and lipid profiles in newly diagnosed hypothyroid patients. Their findings revealed a positive correlation between Hs-CRP and TSH and a significant negative correlation between HDL levels and TSH in hypothyroid patients (30). These results partially align with the observations, except for the HDL levels, which were higher in the hypothyroid patients and showed a non-significant positive correlation with TSH.
The statistical analysis demonstrated positive correlations between TG and VLDL with TSH, while HDL, LDL, and TG exhibited negative correlations with TSH. However, only the negative correlation between LDL and TSH was statistically significant. Additionally, negative correlations were observed between TG, total cholesterol, VLDL, and LDL (excluding HDL) with T3 and T4, though these correlations were not significant.
Conclusion
In this study, positive correlations were observed between Hs-CRP and TSH, T3, and TG, while negative correlations were noted with total cholesterol, VLDL-C, HDL-C, and T4 in hypothyroid subjects. The positive correlation between Hs-CRP and TSH, as well as TG and LDL-C, suggests a potential role for Hs-CRP as a mediator between thyroid disorders and cardiovascular disease. However, further research with larger sample sizes is needed to confirm these findings due to the lack of statistical significance in most of the results, potentially attributed to the smaller sample size compared to other studies.
Acknowledgement
The authors express their gratitude to Mrs. Nahid Poursharifi for her assistance in the experimental aspects of this study.
Funding sources
This project, registered with the Deputy of Research and Technology of Golestan University of Medical Sciences (Gorgan, Iran) under approval number 113232, was funded by Mr. Ameer Abdulraheem Handhal, an MSc student at Golestan University of Medical Sciences.
Ethical statement
Ethical approval for this study was obtained from Golestan University of Medical Sciences (Ethical number IR.GOUMS.REC.1401.565).
Conflicts of interest
The authors declare no conflicts of interest.
Author contributions
Ameer Abdulraheem Handhal: Wrote the proposal and conducted the experimental aspects of the study.
Mahin Gholipur: Collaborated in writing the proposal.
Fatima Mohammadzadeh: Collaborated in the sampling phase of the study.
Somayeh Ghorbani: Performed data analysis.
Safoura Khajeniazi: Supervised the thesis, interpreted results, and wrote the manuscript.
Article Type: Research |
Subject:
Biochemistry
References
1. Li T, Geng H, Wang Y, Wu Z, Yang S, Hu Y. Causal Association of Thyroid Signaling with C-Reactive Protein: A Bidirectional Mendelian Randomization. Hindawi Computational and Mathematical Methods in Medicine. 2022;2022:8954606. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Michalaki MA , Vagenakis AG , Leonardou AS , Argentou MN, Habeos LG, Makri MG, et al. Thyroid function in humans with morbid obesity. Thyroid. 2006;16(1):73-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Biondi B, Cappola AR, Cooper DS. Subclinical hypothyroidism. JAMA. 2019;322(2):153-60. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Rizos CV, Elisaf MS, Liberopoulos EN. Effects of Thyroid Dysfunction on Lipid Profile. Open Cardiovasc Med J. 2011;5:76-84 [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Duntas LH. Thyroid disease and lipids. Thyroid. 2002;12(4):287-93. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Asvold BO, Vatten LJ, Nilsen TI, Bjoro T. The association between TSH within the reference range and serum lipid concentrations in a population-based study. The HUNT Study. Eur J Endocrinol. 2007;156(2):181-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Ahmad N, Iqbal S, Javed M, Ahmad M, Nafees S, Augusthy A. Relationship of Hypothyroidism with Lipid Levels, hs-CRP and BMI. Int J Cur Res Rev. 2021;13(23):104-7. [View at Publisher] [DOI] [Google Scholar]
8. Jose E, Miranda P, Bittencourt M, Santos I , Lotufo P , Benseñor I. Thyroid Function and High-Sensitivity C-Reactive Protein in Cross-Sectional Results from the Brazilian Longitudinal Study of Adult Health. Eur Thyroid J. 2016;5(4):240-6 [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Janssen IM, Homan J, Schijns W, Betzel B , Aarts E , Berends F, et al. Subclinical hypothyroidism and its relation to obesity in patients before and after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015;11(6):1257-63. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. O'Brien T, Dinneen SF, O'Brien PC, Palumbo PJ. Hyperlipidemia in patients with primary and secondary hypothyroidism. Mayo Clin Proc. 1993;68(9):860-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Bensenor IM, Goulart AC, Molina Mdel C, Miranda E , Santos I , Lotufo P. Thyrotropin levels, insulin resistance, and metabolic syndrome: a cross-sectional analysis in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Metab Syndr Relat Disord. 2015;13(8):362-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Albert MA , Danielson E, Rifai N, Ridker PM. Effect of statin therapy on C-reactive protein levels; the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA. 2001;286(1):64-70. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Czarnywojtek A, Owecki M, Zgorzalewicz-Stachowiak M, Woliński K, Szczepanek-Parulska E, Budny B. The Role of Serum C-Reactive Protein Measured by High-Sensitive Method in Thyroid Disease. Arch Immunol Ther Exp. 2014;62:501-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Tuzcu A, Bahceci M, Gokalp D, Tuzun Y, Gunes K. Subclinical Hypothyroidism may be associated with elevated High-sensitive C-reactive protein (low grade inflammation) And fasting hyperinsulinemia. Endocr J. 2005;52(1):89-94. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Ganesan A, Sethulekshmi S, et al: Relationship between hs-CRP and TSH in patients with subclinical hypothyroidism. Rom J Diabetes Nutr Metab Dis. 2021;28(4):391-4. [View at Publisher] [DOI] [Google Scholar]
16. Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of CRP and LDL cholesterol in prediction of first cardiovascular event. N Engl J Med. 2002;347(20):1557-65. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Sharma P, Prashar N, Sharma G, Singh H, Sharma R. Lipid profile and hs-CRP levels in patients with subclinical hypothyroidism. Int J Med Sci Public Health. 2016;5(6):1233-6. [View at Publisher] [DOI] [Google Scholar]
18. Christ-Crain M, Meier C, Guglielmetti M, Huber PR, Riesen W, Staub JJ, et al. Elevated C-reactive protein and homocytsteine values: cardiovascular risk factors in hypothyroidism? A cross-sectional and double blind, placebo controlled trial. Atherosclerosis. 2003;166(2):379-86. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Jung CH, Sung KC, Shin HS, Rhee EJ, Lee WY, Kim BS, et al. Thyroid dysfunction to cardiovascular risk factors such as lipid profile, hs-CRP and waist hip ratio in Korea. Korean J Intern Med. 2003;18(3):146-53. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Shantha G, Kumar A, Jeyachandran V, Rajamanickam D, Rajkumar K, Salim S, et al. Association between primary hypothyroidism and metabolic syndrome and the role of C reactive protein. Thyroid Research. 2009;2(2):1-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Krishnamurthy H, Ravitej S. Predictive Significance of High-Sensitive C-reactive Protein in Subclinical Hypothyroidism. J Clin Diagn Res. 2022;16(10):15-7. [View at Publisher] [DOI] [Google Scholar]
22. Ahmad N, Nagtilak S, Sharma A, Parashar P, Rastogi A. Role of Circulating C-Reactive Protein in Thyroid Disorders. JMSCR. 2018;06(02):485-9. [View at Publisher] [DOI] [Google Scholar]
23. Sharma R, Sharma TK, Kaushik GG, Sharma S, Vardey SK, Sinha M. Subclinical hypothyroidism and its association with cardiovascular risk factors.Clin Lab. 2011;57(9-10):719-24. [View at Publisher] [DOI] [Google Scholar]
24. Ahmad N, Ahmad M, Gupta A, Sharma AK. Association of Elevated Serum hs-CRP Levels with the Development of Cardiovascular Disease in Known Cases of Hypothyroidism: A case-control study. National Journal of Laboratory Medicine. 2022;11(1):16-9. [View at Publisher] [DOI] [Google Scholar]
25. Kshetrimayum V, Usha SMR, Vijayalakshmi P. A study of hs-CRP and lipid profile in hypothyroid adults at tertiary care hospital. International Journal of Clinical Biochemistry and Research. 2019;6(3):303-10. [View at Publisher] [DOI] [Google Scholar]
26. Wang C. The Relationship between Type 2 Diabetes Mellitus and Related Thyroid Diseases. J Diabetes Res. 2013;2013:390534. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Jublanc C, Bruckert E, Giral P, Chapman MJ, Leenhardt L, Carreau V , et al. Relationship of circulating C-reactive protein levels to thyroid status and cardiovascular risk in hyperlipidemic euthyroid subjects: low free thyroxine is associated with elevated hs-CRP. Atherosclerosis. 2004;172(1):7-11. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Rustam S, Hassan B. Assessment of inflammatory marker (Hs-CRP and OPN) and other parameters in Hypothyroidism. Teikyo Medical Journal. 2021;44(6):2325-31. [View at Publisher] [Google Scholar]
29. Jha U, et al: To Compare the Thyroid Profile, hs-CRP, and Lipid Profile in Newly Diagnosed Hypothyroid Adults to Controls, as well as to Compare the above Parameters in Subclinical and Clinical Hypothyroid Instances. European Journal of Molecular & Clinical Medicine (EJMCM). 2021; 4: 2515-8260. [Google Scholar]
30. Sumanth Kumar B, Sampson U, Pratheeba J, Ponnazhagan K. Study of Vitamin D, hs-CRP and Lipid Profile Status in Newly Diagnosed. Hypothyroid Patients in the Local Population of Kanchipuram District. Sch Int J Biochem. 2020;3(9):201-5. [View at Publisher] [DOI]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).



