Volume 8, Issue 2 (Journal of Clinical and Basic Research (JCBR) 2024)
jcbr 2024, 8(2): 20-23 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hameed A A, Kudalkar U N, Madhale N R. Supracondylar process of the humerus - A Morphometric Study. jcbr 2024; 8 (2) :20-23
URL: http://jcbr.goums.ac.ir/article-1-443-en.html
URL: http://jcbr.goums.ac.ir/article-1-443-en.html
1- Department of Anatomy, Goa Medical College & Hospital, Bambolim, Goa, India , aliahameedmbbs@gmail.com
2- Department of Anatomy, Goa Medical College & Hospital, Bambolim, Goa, India
2- Department of Anatomy, Goa Medical College & Hospital, Bambolim, Goa, India
Full-Text [PDF 446 kb]
(992 Downloads)
| Abstract (HTML) (2368 Views)
Full-Text: (745 Views)
Introduction
The supracondylar process of the humerus, also referred to as the supra-epitrochlear process or supracondylar spur, is a bony protrusion resembling a hook that varies in size and extends distally from the front inner surface of the humerus. It is situated approximately 5 cm proximal to the medial epicondyle, with a length ranging from 2 mm to 20 mm. This process may be connected to the medial epicondyle by a fibrous band known as the ligament of Struthers, to which a portion of the pronator teres muscle is attached. Together, the band, the process, and the shaft of the humerus form a ring through which the median nerve and the brachial artery (Or one of its branches) may pass (1). The ligament of Struthers corresponds to the third head of the coracobrachialis (2). Compression of the brachial artery or the median nerve in this area may lead to supracondylar process syndrome. Struthers, Solieri and Aydinlioglu et al. (3,4) have documented cases of median nerve compression. Talha et al. (5), and Thompson and Edwards (6) have reported compression and claudication of the brachial artery. Furthermore, Spinner (7) has documented fractures of the supracondylar process.
The first depiction of a supracondylar process can be found in ‘Tiedmann’s Tabulae Arterium’(8). The incidence of this condition varies from 0.1% to 2.7% (9). According to Kessel and Ring (10), the ligament of Struthers represents the tendon of a vestigial muscle, the latissimo-condyloideus, present in marsupials, reptiles, cats, lemurs and American monkeys. Limited research has been conducted on the supracondylar process in the Indian population thus far (11-16). The primary objective of this study is to determine the prevalence of the supracondylar process of the humerus in individuals of South Indian descent and to discuss its clinical significance.
Methods
The study focused on examining 83 dried humeri from the osteological collection in the Department of Anatomy at Goa Medical College in Bambolim, Goa, India. This anatomical research was conducted under ethical guidelines, having received approval from the Institutional Ethics Committee of Goa Medical College (Approval number GMCIEC/2023/238) on July 15, 2023.
To identify and analyze the supracondylar process the bones were thoroughly inspected under natural light conditions. The inspection process involved a detailed examination of each humerus to detect the presence of any bony protrusions or abnormalities that could indicate a supracondylar process. Upon identifying a supracondylar process, precise measurements were taken using a digital Vernier Caliper. The measurements included parameters such as the length of the supracondylar process, the breadth at its base, and its distance from specific anatomical landmarks, like the medial epicondyle and nutrient foramen. Additionally, photographs of the supracondylar process were taken to provide a visual record of the findings and assist in further analysis.
Results
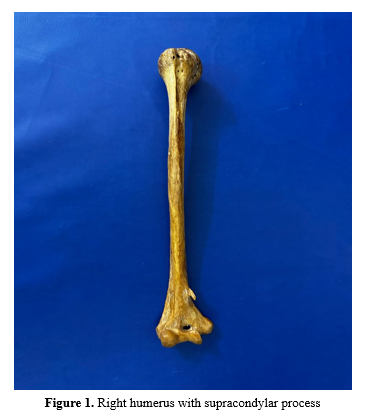
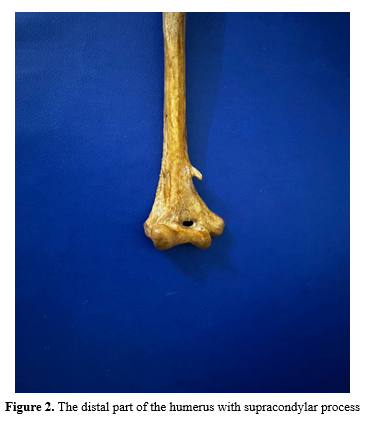
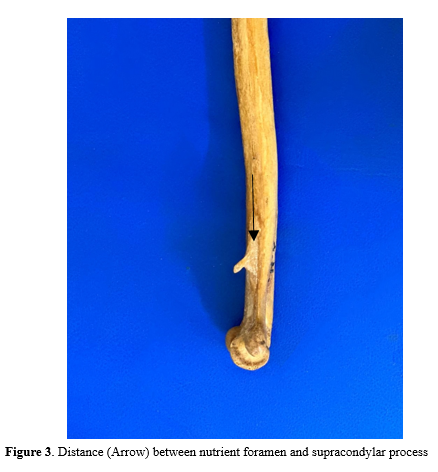
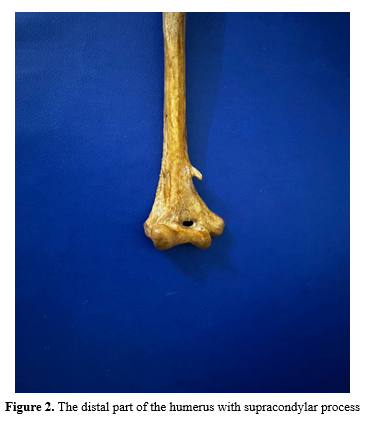
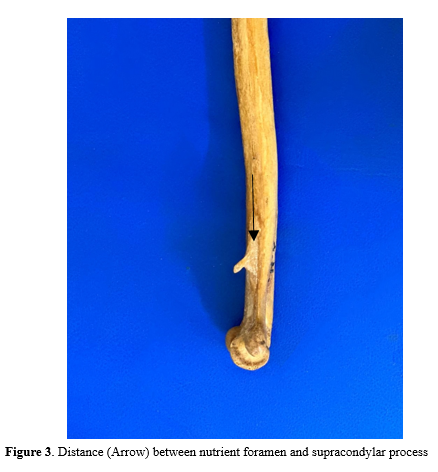
In our examination of 83 dried humeri, we observed a singular instance of a right humerus bearing a supracondylar process on its anteromedial surface (Figure 1 and 2). This process was located 4.4 cm proximal to the medial epicondyle, protruding 1.1 cm from the surface, with a base measuring 1.1 cm in length and 1 cm in width. The spine of the process extended downwards, forwards, and medially, with the distance from its tip to the medial supracondylar ridge measuring 4.4 cm. Additionally, the base of the spine was situated 4.7 cm from the nutrient foramen (Figure. 3). The overall length of this humerus, from the lowest tip of the trochlea to the highest point of the head, was 28.7 cm.
Comparing the present study with previous studies on the measurements of the supracondylar process in the Indian population, we observe several similarities and differences across four key parameters: the length of the spine, breadth at the base of the spine, distance of the spine from the medial epicondyle, and distance of the spine from the nutrient foramen (Table 1).
Length of spine:
The present study reports a length of 1.1 cm, consistent with the findings of Baruah et al. (14) and Nikumbh et al. (16) However, Gupta and Mehta(12) reported a significantly shorter length of 0.3 cm, while Shivaleela et al. (13) and Vandana and Patil (15) reported lengths of 1.0 cm and 0.8 cm, respectively.
Breadth at the base of the spine:
The breadth reported in the present study is 1.0 cm, matching the findings of Shivaleela et al. (13) and Nikumbh et al. (16) In contrast, Gupta and Mehta (12) and Vandana and Patil (15) reported slightly wider measurements of 1.1 cm and 1.2 cm, respectively. Baruah et al. (14) reported the broadest measurement at 1.5 cm.
Distance of spine from medial epicondyle:
The present study reports a distance of 4.4 cm, which is consistent with Baruah et al. (14) but shorter than the measurements reported by other studies. Gupta and Mehta (12) reported a distance of 6.5 cm, Shivaleela et al. (13) 6.0 cm, Vandana and Patil (15) 5.3 cm, and Nikumbh et al. (16) 5.5 cm.
Distance of spine from nutrient foramen:
The present study reports a distance of 4.7 cm, which matches the findings of Shivaleela et al. (13) However, this measurement is shorter compared to Baruah et al. (14) and Nikumbh et al. (16), who reported 6.5 cm, and Vandana and Patil (15), who reported 5.5 cm.
Overall, while there is consistency in some measurements, such as the breadth at the base of the spine, significant variability is seen in the length of the spine and the distances from the medial epicondyle and nutrient foramen.
The present study reports an incidence of 1.2% for the supracondylar process in the Indian population from Goa. This rate is relatively higher compared to several previous studies conducted within India and aligns more closely with rates observed in certain non-Indian populations (Table 2).
Comparatively, Gupta and Mehta (12) found a much lower incidence of 0.26% in Indians from Gujarat, while Baruah et al. (14) reported an incidence of 1.25% in Indians from Assam, which is very close to the rate observed in the present study. Shivaleela et al. (13) reported a 0.41% incidence in Indians from Karnataka, and Nikumbh et al. (16) observed a 0.36% incidence in Indians from Maharashtra, both of which are lower than the present study's findings.
The incidence rates also vary in international contexts, Gruber (1865) reported a higher incidence of 2.7% in the European race, whereas Hrdliyka (1923) found a 1% incidence among American Indians, which is slightly lower than in the present study. Danforth (1924) and Adachi (1928) reported incidences of 0.5% and 0.8% respectively in mixed populations, which are also lower than the present study's rate. Terry (1930) observed a 0.1% incidence in blacks and 1.16% in Europeans, with the latter being comparable to the present study's findings. Parkinson (17) reported a 0.4% incidence in a mixed population, much lower than the present study. Dellon (18) observed a 1.15% incidence in Europeans, similar to the present study's findings. Oluyemi (19) reported a significantly higher incidence of 2.5% in Nigerians, and Natsis (20) found a 1.3% incidence in Caucasians, slightly higher than the present study.
Overall, the incidence of the supracondylar process varies widely both within and across different populations and ethnic groups. The 1.2% incidence rate found in the present study is notably higher than most reported in other Indian studies but falls within the range observed in some international populations, particularly among Europeans and Caucasians. This variability may be attributed to genetic, environmental, or methodological factors influencing the detection and reporting of the supracondylar process.
Discussion
The knowledge of anatomical variations is important to anatomists, radiologists, anaesthesiologists and surgeons in modern diagnostic medicine. Morphological differences are the tools to find the missing links between different stages of evolution. One such variation is the supracondylar process of the humerus.
The incidence of supracondylar process is usually very low. In ‘Cornelia de Lange syndrome’, an autosomal recessive trait, there is a high incidence of unilateral supracondylar process of the humerus, occurring in approximately one in every 10,000 live births (21). Though usually clinically silent, it may become symptomatic by presenting as a mass or associated with symptoms of median nerve compression and brachial artery claudication.
Entrapment of brachial artery and median nerve by Struthers’ ligament at the level of supracondylar process is known as supracondylar process syndrome which is treated by surgical removal of the ligament and the process along with underlying periosteum to prevent recurrence (17). The compression symptoms include ischemic pain of the forearm, severe paraesthesia and hyperesthesia of the hand and fingers, embolization of the distal arm arteries and disappearance of the radial or ulnar pulse on full extension and supination of forearm (22). Rarely, ulnar nerve compression can also occur if the Struthers’ ligament, instead of being attached to the medial epicondyle, extends downward as a band that blends with the fibrous arch between the two heads of flexor carpi ulnaris (23,24). A supracondylar process may be misdiagnosed as an osteochondroma. The process is oriented distally towards the elbow joint and there is no discontinuity in the cortex of the humerus in X-ray, whereas an osteochondroma points away from the joint and the cortex of the tumor is continuous with the humeral cortex. Heterotopic bone such as myositis ossificans can also mimic a supracondylar process (25).
The supracondylar process measurements exhibit variability among different studies. This could be due to differences in the sample sizes, demographic variations within the Indian population, or methodological differences in the studies. Despite these differences, some consistency is observed in measurements like the breadth at the base of the spine.
These measurements are crucial in clinical settings, especially in surgeries involving the humerus, as the supracondylar process can be a site of muscle and ligament attachment and may also affect nerve positioning. Understanding the variations in its anatomy is important for clinicians to avoid complications.
Conclusion
The supracondylar process, though usually clinically silent, may present as a mass or symptoms of median nerve compression and brachial artery claudication. Hence its knowledge becomes important to anatomists, radiologists, as well as surgeons to avoid misdiagnosis. The present study reports a 1.2% incidence of the supracondylar process in the Indian population of Goa, which is relatively high compared to other Indian studies. This suggests regional variations within India, potentially influenced by genetic, environmental, or methodological factors. The higher incidence in Goa highlights the need for further research to understand the underlying reasons for these regional differences in the prevalence of the supracondylar process.
Acknowledgement
The authors sincerely show gratitude to those who donated their bodies to science so that anatomical research could be performed.
Funding sources
None.
Ethical statement
This study was approved by the Institutional Ethics Committee of Goa Medical College, Bambolim (GMCIEC/2023/238) on 2023/07/15.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
Ali Abdul Hameed and Uday Narayan Kudalkar: conceptualization; Ali Abdul Hameed: writing-original draft; Uday Narayan Kudalkar and Nilam Rajesh Madhale: writing-review and editing. All authors read and approved the final manuscript.
The supracondylar process of the humerus, also referred to as the supra-epitrochlear process or supracondylar spur, is a bony protrusion resembling a hook that varies in size and extends distally from the front inner surface of the humerus. It is situated approximately 5 cm proximal to the medial epicondyle, with a length ranging from 2 mm to 20 mm. This process may be connected to the medial epicondyle by a fibrous band known as the ligament of Struthers, to which a portion of the pronator teres muscle is attached. Together, the band, the process, and the shaft of the humerus form a ring through which the median nerve and the brachial artery (Or one of its branches) may pass (1). The ligament of Struthers corresponds to the third head of the coracobrachialis (2). Compression of the brachial artery or the median nerve in this area may lead to supracondylar process syndrome. Struthers, Solieri and Aydinlioglu et al. (3,4) have documented cases of median nerve compression. Talha et al. (5), and Thompson and Edwards (6) have reported compression and claudication of the brachial artery. Furthermore, Spinner (7) has documented fractures of the supracondylar process.
The first depiction of a supracondylar process can be found in ‘Tiedmann’s Tabulae Arterium’(8). The incidence of this condition varies from 0.1% to 2.7% (9). According to Kessel and Ring (10), the ligament of Struthers represents the tendon of a vestigial muscle, the latissimo-condyloideus, present in marsupials, reptiles, cats, lemurs and American monkeys. Limited research has been conducted on the supracondylar process in the Indian population thus far (11-16). The primary objective of this study is to determine the prevalence of the supracondylar process of the humerus in individuals of South Indian descent and to discuss its clinical significance.
Methods
The study focused on examining 83 dried humeri from the osteological collection in the Department of Anatomy at Goa Medical College in Bambolim, Goa, India. This anatomical research was conducted under ethical guidelines, having received approval from the Institutional Ethics Committee of Goa Medical College (Approval number GMCIEC/2023/238) on July 15, 2023.
To identify and analyze the supracondylar process the bones were thoroughly inspected under natural light conditions. The inspection process involved a detailed examination of each humerus to detect the presence of any bony protrusions or abnormalities that could indicate a supracondylar process. Upon identifying a supracondylar process, precise measurements were taken using a digital Vernier Caliper. The measurements included parameters such as the length of the supracondylar process, the breadth at its base, and its distance from specific anatomical landmarks, like the medial epicondyle and nutrient foramen. Additionally, photographs of the supracondylar process were taken to provide a visual record of the findings and assist in further analysis.
Results
In our examination of 83 dried humeri, we observed a singular instance of a right humerus bearing a supracondylar process on its anteromedial surface (Figure 1 and 2). This process was located 4.4 cm proximal to the medial epicondyle, protruding 1.1 cm from the surface, with a base measuring 1.1 cm in length and 1 cm in width. The spine of the process extended downwards, forwards, and medially, with the distance from its tip to the medial supracondylar ridge measuring 4.4 cm. Additionally, the base of the spine was situated 4.7 cm from the nutrient foramen (Figure. 3). The overall length of this humerus, from the lowest tip of the trochlea to the highest point of the head, was 28.7 cm.
Comparing the present study with previous studies on the measurements of the supracondylar process in the Indian population, we observe several similarities and differences across four key parameters: the length of the spine, breadth at the base of the spine, distance of the spine from the medial epicondyle, and distance of the spine from the nutrient foramen (Table 1).
|
Table 1. Measurements of supracondylar process in Indian population reported by different authors
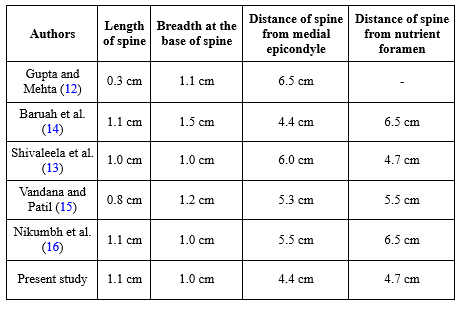 |
The present study reports a length of 1.1 cm, consistent with the findings of Baruah et al. (14) and Nikumbh et al. (16) However, Gupta and Mehta(12) reported a significantly shorter length of 0.3 cm, while Shivaleela et al. (13) and Vandana and Patil (15) reported lengths of 1.0 cm and 0.8 cm, respectively.
Breadth at the base of the spine:
The breadth reported in the present study is 1.0 cm, matching the findings of Shivaleela et al. (13) and Nikumbh et al. (16) In contrast, Gupta and Mehta (12) and Vandana and Patil (15) reported slightly wider measurements of 1.1 cm and 1.2 cm, respectively. Baruah et al. (14) reported the broadest measurement at 1.5 cm.
Distance of spine from medial epicondyle:
The present study reports a distance of 4.4 cm, which is consistent with Baruah et al. (14) but shorter than the measurements reported by other studies. Gupta and Mehta (12) reported a distance of 6.5 cm, Shivaleela et al. (13) 6.0 cm, Vandana and Patil (15) 5.3 cm, and Nikumbh et al. (16) 5.5 cm.
Distance of spine from nutrient foramen:
The present study reports a distance of 4.7 cm, which matches the findings of Shivaleela et al. (13) However, this measurement is shorter compared to Baruah et al. (14) and Nikumbh et al. (16), who reported 6.5 cm, and Vandana and Patil (15), who reported 5.5 cm.
Overall, while there is consistency in some measurements, such as the breadth at the base of the spine, significant variability is seen in the length of the spine and the distances from the medial epicondyle and nutrient foramen.
The present study reports an incidence of 1.2% for the supracondylar process in the Indian population from Goa. This rate is relatively higher compared to several previous studies conducted within India and aligns more closely with rates observed in certain non-Indian populations (Table 2).
|
Table 2. The incidence of supracondylar process reported in studies of different races
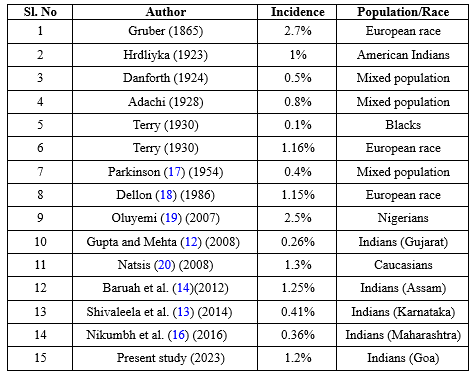 |
The incidence rates also vary in international contexts, Gruber (1865) reported a higher incidence of 2.7% in the European race, whereas Hrdliyka (1923) found a 1% incidence among American Indians, which is slightly lower than in the present study. Danforth (1924) and Adachi (1928) reported incidences of 0.5% and 0.8% respectively in mixed populations, which are also lower than the present study's rate. Terry (1930) observed a 0.1% incidence in blacks and 1.16% in Europeans, with the latter being comparable to the present study's findings. Parkinson (17) reported a 0.4% incidence in a mixed population, much lower than the present study. Dellon (18) observed a 1.15% incidence in Europeans, similar to the present study's findings. Oluyemi (19) reported a significantly higher incidence of 2.5% in Nigerians, and Natsis (20) found a 1.3% incidence in Caucasians, slightly higher than the present study.
Overall, the incidence of the supracondylar process varies widely both within and across different populations and ethnic groups. The 1.2% incidence rate found in the present study is notably higher than most reported in other Indian studies but falls within the range observed in some international populations, particularly among Europeans and Caucasians. This variability may be attributed to genetic, environmental, or methodological factors influencing the detection and reporting of the supracondylar process.
Discussion
The knowledge of anatomical variations is important to anatomists, radiologists, anaesthesiologists and surgeons in modern diagnostic medicine. Morphological differences are the tools to find the missing links between different stages of evolution. One such variation is the supracondylar process of the humerus.
The incidence of supracondylar process is usually very low. In ‘Cornelia de Lange syndrome’, an autosomal recessive trait, there is a high incidence of unilateral supracondylar process of the humerus, occurring in approximately one in every 10,000 live births (21). Though usually clinically silent, it may become symptomatic by presenting as a mass or associated with symptoms of median nerve compression and brachial artery claudication.
Entrapment of brachial artery and median nerve by Struthers’ ligament at the level of supracondylar process is known as supracondylar process syndrome which is treated by surgical removal of the ligament and the process along with underlying periosteum to prevent recurrence (17). The compression symptoms include ischemic pain of the forearm, severe paraesthesia and hyperesthesia of the hand and fingers, embolization of the distal arm arteries and disappearance of the radial or ulnar pulse on full extension and supination of forearm (22). Rarely, ulnar nerve compression can also occur if the Struthers’ ligament, instead of being attached to the medial epicondyle, extends downward as a band that blends with the fibrous arch between the two heads of flexor carpi ulnaris (23,24). A supracondylar process may be misdiagnosed as an osteochondroma. The process is oriented distally towards the elbow joint and there is no discontinuity in the cortex of the humerus in X-ray, whereas an osteochondroma points away from the joint and the cortex of the tumor is continuous with the humeral cortex. Heterotopic bone such as myositis ossificans can also mimic a supracondylar process (25).
The supracondylar process measurements exhibit variability among different studies. This could be due to differences in the sample sizes, demographic variations within the Indian population, or methodological differences in the studies. Despite these differences, some consistency is observed in measurements like the breadth at the base of the spine.
These measurements are crucial in clinical settings, especially in surgeries involving the humerus, as the supracondylar process can be a site of muscle and ligament attachment and may also affect nerve positioning. Understanding the variations in its anatomy is important for clinicians to avoid complications.
Conclusion
The supracondylar process, though usually clinically silent, may present as a mass or symptoms of median nerve compression and brachial artery claudication. Hence its knowledge becomes important to anatomists, radiologists, as well as surgeons to avoid misdiagnosis. The present study reports a 1.2% incidence of the supracondylar process in the Indian population of Goa, which is relatively high compared to other Indian studies. This suggests regional variations within India, potentially influenced by genetic, environmental, or methodological factors. The higher incidence in Goa highlights the need for further research to understand the underlying reasons for these regional differences in the prevalence of the supracondylar process.
Acknowledgement
The authors sincerely show gratitude to those who donated their bodies to science so that anatomical research could be performed.
Funding sources
None.
Ethical statement
This study was approved by the Institutional Ethics Committee of Goa Medical College, Bambolim (GMCIEC/2023/238) on 2023/07/15.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
Ali Abdul Hameed and Uday Narayan Kudalkar: conceptualization; Ali Abdul Hameed: writing-original draft; Uday Narayan Kudalkar and Nilam Rajesh Madhale: writing-review and editing. All authors read and approved the final manuscript.
Article Type: Research |
Subject:
Basic medical sciences
References
1. Williams PL, Warwick R, Dyson M, Bannister LH, editors. In: Gray's Anatomy. 39th ed. Edinburgh London:Churchill Livingstone;2005. p.850. [View at Publisher] [Google Scholar]
2. Datta AK. Essentials of human anatomy. In: Superior and inferior extremity. 5th ed. Kolkata:Current Books International;2017. p.49. [View at Publisher] [Google Scholar]
3. Solieri SA. Nervalgia del nervo mediano da processo sopraepitrocleare. Chir Organi Mov. 1929;14:71. [Google Scholar]
4. Aydinlioglu A, Cirak B, Akpinar F, Tosun N, Dogan A. Bilateral median nerve compression at the level of Struthers' ligament. J Neurosurg. 2000;92(4):693-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Talha H, Enon B, Chevalier JM, L'Hoste P, Pillet J. Brachial artery entrapment: compression by the supracondylar process. Ann Vasc Surg. 1987;1(4):479-82. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Thompson JK, Edwards JD. Supracondylar Process of the Humerus Causing Brachial Artery Compression and Digital Embolization in a Fast-Pitch Softball Player: A Case Report. Vasc Endovascular Surg. 2005;39(5):445-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Spinner RJ, Lins RE, Jacobson SR, Nunley JA. Fractures of the supracondylar process of the humerus. J Hand Surg Am. 1994;19(6):1038-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Tiedmann F. Tabulae arterium corporis humani. Karlsruhe:Muller;1822. [View at Publisher] [Google Scholar]
9. Martin-Schütz GO, Arcoverde M, Barros GD, Babinski MA, Manaia JH, Silva CR, et al. A meta-analysis of the supracondylar process of the humerus with clinical and surgical applications to orthopedics. Int j morphol. 2019;37(1):43-8. [View at Publisher] [DOI] [Google Scholar]
10. Kessel L, Rang M. Supracondylar spur of the humerus. J Bone Joint Surg Br. 1966;48(4):765-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Shantharam V, Raghavendra R, Ganesh V. Study of incidence of the supracondylar spur of the humerus among south Indians. Medpulse Int J Anat. 2021;17(3):35-7. [View at Publisher] [DOI]
12. Gupta RK, Mehta CD. A study of the incidence of supracondylar process of the humerus. J Anat Soc. 2008;57(2):111-15. [Google Scholar]
13. Shivaleela C, Suresh BS, Kumar GV, Lakshmiprabha S. Morphological study of the supracondylar process of the humerus and its clinical implications. J Clin Diagn Res. 2014;8(1):1-3. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Baruah P, Choudhury PR, KL Talukdar. A study of supracondylar process of humerus. J Evol Med Dent Sci. 2012;1(5):817-22. [View at Publisher] [DOI]
15. Vandana R, Patil SP. Study of supracondylar process of humerus. Int J Health Allied Sci. 2014;3(2):134-6. [View at Publisher] [DOI] [Google Scholar]
16. Nikumbh RD, Nikumbh DB, Doshi MA, Ugadhe MN, et al. MORPHOMETRIC STUDY OF THE SUPRACONDYLAR PROCESS OF THE HUMERUS WITH ITS CLINICAL UTILITY. Int J Anat Res. 2016;4(1):1941-4. [View at Publisher] [DOI] [Google Scholar]
17. Parkinson CE. The supracondyloid process. Radiology. 1954;62(4):556-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Dellon AL. Musculotendinous variations about the medial humeral epicondyle. J Hand Surg Br. 1986;11(2):175-81. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Oluyemi KA, Okwuonu UC, Adesanya OA, Akinola OB, Ofusori DA, Ukwenya VO, et al. Supracondylar and infratubercular processes observed in the humeri of Nigerians. African Journal of Biotechnology. 2007;6(21):2439-41. [View at Publisher] [DOI] [Google Scholar]
20. Natsis K. Supracondylar process of the humerus: Study on 375 Caucasian subjects in Cologne, Germany. Clin Anat. 2008;21(2):138-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Kuchinka J, Kuder T, Szczurkowski A, Nowak E, Gliński W, Kwieciński J. Rare morphological variants of the bones: epicondylar processes, metopic suture and Wormian bones in XVIII century skeleton. Folia Morphol (Warsz).2020;79(1):162-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Aragão JA, Prado MLDL, Sant'Anna Aragão IC, Sant'Anna Aragão FM, Reis FP, Mendonça DMFD. Case Report on a Supracondylar Process of the Humerus: Morphological and Morphometric analysis. Braz J Case Rep. 2024;4(4):50-6. [View at Publisher] [DOI] [Google Scholar]
23. May-Miller P, Robinson S, Sharma P, Shahane S. The Supracondylar Process: A Rare Case of Ulnar Nerve Entrapment and Literature Review. J Hand Microsurg. 2019;11(Suppl 1):S06-10. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Mittal RL, Gupta BR. Median and ulnar-nerve palsy: an unusual presentation of the supracondylar process. Report of a case.J Bone Joint Surg Am. 1978;60(4):557-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Airon D, Airon N, Jain P, Jain A, Airon A. Supracondylar Process of Humerus - Report of Two Cases. J Evol Med Dent Sci. 2022;11(7):710-1. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






