Volume 7, Issue 4 (Journal of Clinical and Basic Research (JCBR) 2023)
jcbr 2023, 7(4): 10-14 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shaik M B, Mallam K K, Vurundhur D, Talari A B. A study of relapse rate and functional outcome after surgical debridement in patients with chronic osteomyelitis. jcbr 2023; 7 (4) :10-14
URL: http://jcbr.goums.ac.ir/article-1-429-en.html
URL: http://jcbr.goums.ac.ir/article-1-429-en.html
1- Department of Orthopaedics, ACSR Govt Medical College, Nellore, Andhra Pradesh, India , bonesbasha@gmail.com
2- Department of Orthopaedics, ACSR Govt Medical College, Nellore, Andhra Pradesh, India
2- Department of Orthopaedics, ACSR Govt Medical College, Nellore, Andhra Pradesh, India
Keywords: Osteomyelitis, Debridement, Emotional status, Functional outcome, Relapse rate, Musculoskeletal Tumour Society
Full-Text [PDF 514 kb]
(142 Downloads)
| Abstract (HTML) (425 Views)

Full-Text: (47 Views)
Introduction
Chronic osteomyelitis is caused by untreated or incompletely treated hematogenous osteomyelitis, untreated open fractures, or surgical infection complications. Recurrence with the same organism isolate is referred to as "relapse," while recurrence with a different or extra strain is referred to as "re-infection" (1).
There has also been a continual evolution in diagnostic techniques, novel antibiotics, biomaterials, and reconstructive operations (2).
Antibiotic therapy alone will not suffice due to its poor kinetics in bone with sequestrae and fistulae. Currently, surgical debridement is the preferred method, with minimum or no systemic antibiotics and/or local antibiotics (3,4).
The most difficult aspect of treating chronic osteomyelitis is that infection eradication is a major concern. Various patients relapse over time, necessitating several operations and lengthy hospitalizations, imposing a significant financial burden on patients and health care systems (5). Chronic osteomyelitis had a recurrence rate ranging from 0% to 48% (6,7,8). The emotional, physical, and financial burdens associated with chronic osteomyelitis have had a profound impact on the lives of millions of individuals worldwide (9).
A significant number of studies and new research continue to be conducted in the diagnosis and management of osteomyelitis. There is very little research on the functional result and relapse rates after surgery.
Chronic osteomyelitis is caused by untreated or incompletely treated hematogenous osteomyelitis, untreated open fractures, or surgical infection complications. Recurrence with the same organism isolate is referred to as "relapse," while recurrence with a different or extra strain is referred to as "re-infection" (1).
There has also been a continual evolution in diagnostic techniques, novel antibiotics, biomaterials, and reconstructive operations (2).
Antibiotic therapy alone will not suffice due to its poor kinetics in bone with sequestrae and fistulae. Currently, surgical debridement is the preferred method, with minimum or no systemic antibiotics and/or local antibiotics (3,4).
The most difficult aspect of treating chronic osteomyelitis is that infection eradication is a major concern. Various patients relapse over time, necessitating several operations and lengthy hospitalizations, imposing a significant financial burden on patients and health care systems (5). Chronic osteomyelitis had a recurrence rate ranging from 0% to 48% (6,7,8). The emotional, physical, and financial burdens associated with chronic osteomyelitis have had a profound impact on the lives of millions of individuals worldwide (9).
A significant number of studies and new research continue to be conducted in the diagnosis and management of osteomyelitis. There is very little research on the functional result and relapse rates after surgery.
The primary objective of this study was to fill a knowledge gap by investigating the rate of relapse after surgical intervention. Additionally, the study aimed to evaluate the functional outcome of patients who underwent surgical debridement. Furthermore, the researchers aimed to describe the rate of recurrence or relapse of chronic osteomyelitis following surgical debridement and compare the functional outcomes during regular follow-up visits.
Methods
Patients who were diagnosed with chronic osteomyelitis based on clinical, radiological, or culture evidence and underwent surgical debridement were included in the study.
Chronic osteomyelitis-host type A and B (Cierny and Mader) patients were studied.
The study was carried out in the Department of Orthopaedics at ACSR Govt Medical College in Nellore, Andhra Pradesh.
All patients with single long bone osteomyelitis or infected non-:union:, adults over the age of 18yrs, patients who had surgical debridement, and patients with a minimum follow-up of 3 months were included (Figure 1).
Exclusion criteria were patients with multifocal osteomyelitis, joint involvement, vascular compromise, Type C host, and bone loss (lengthening/bone transport).
Methods
Patients who were diagnosed with chronic osteomyelitis based on clinical, radiological, or culture evidence and underwent surgical debridement were included in the study.
Chronic osteomyelitis-host type A and B (Cierny and Mader) patients were studied.
The study was carried out in the Department of Orthopaedics at ACSR Govt Medical College in Nellore, Andhra Pradesh.
All patients with single long bone osteomyelitis or infected non-:union:, adults over the age of 18yrs, patients who had surgical debridement, and patients with a minimum follow-up of 3 months were included (Figure 1).
Exclusion criteria were patients with multifocal osteomyelitis, joint involvement, vascular compromise, Type C host, and bone loss (lengthening/bone transport).

Procedure
Patients were divided into groups based on whether or not a preoperative magnetic resonance imaging (MRI) was performed, and relapse rates were compared. Data were gathered from patients suffering from chronic osteomyelitis of the long bones. The Association for the Study and Application of the Method of Ilizarov Criteria (ASAMI), Musculoskeletal Tumor Society (MSTS-functional category), and Lower Extremity Functional Scale (LEFS) for lower limb long bone osteomyelitis, and Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaires for upper limb long bone osteomyelitis were used to track patients' functional outcomes.
Diagnosis
The relapse of chronic osteomyelitis was described as an infection arising again at the same spot from which it was previously thought to be cleared and which was specifically treated with surgery. On presentation, the infection is described as the growth of the same pathogen or a new pathogen in repeat cultures.
Follow-up
Patients were divided into groups based on whether or not a preoperative magnetic resonance imaging (MRI) was performed, and relapse rates were compared. Data were gathered from patients suffering from chronic osteomyelitis of the long bones. The Association for the Study and Application of the Method of Ilizarov Criteria (ASAMI), Musculoskeletal Tumor Society (MSTS-functional category), and Lower Extremity Functional Scale (LEFS) for lower limb long bone osteomyelitis, and Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaires for upper limb long bone osteomyelitis were used to track patients' functional outcomes.
Diagnosis
The relapse of chronic osteomyelitis was described as an infection arising again at the same spot from which it was previously thought to be cleared and which was specifically treated with surgery. On presentation, the infection is described as the growth of the same pathogen or a new pathogen in repeat cultures.
Follow-up
A patient was termed relapse-free if there were no clinical symptoms of infection such as warmth, discharging sinus, fever, edema, or soreness during follow-up. The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were used to confirm normalization. Participants were followup of minimum of 3months and maximum upto 9 months from February 2023 to October 2023. Study duration is Preoperative MRI or infected non-:union:/chronic osteomyelitis classified patients into groups.
The relapse is defined as the recurrence of infection in the same location where it was previously thought to be cleared and was particularly treated with surgery.
Statistical analysis
Demographic, clinical, and laboratory characteristics were all documented in a proforma. An analysis of variance (ANOVA) was performed to analyze continuous variables with preoperative frequency data. Chi-square tests were used to examine categorical variables that had a functional consequence. Non-categorical results were compared using a Student’s t-test. The relationship between the score and clinical profile was assessed using Pearson correlation analysis. P values less than 0.05 were considered statistically significant. Statistical analysis was done using SPSS version 22.0.
Results
Among the 100 patients, 60 had chronic osteomyelitis, and 40 had infected non-:union:. The average age was 35 years. Males made up 82% of the patients.
The majority of patients (82%) were diagnosed with chronic osteomyelitis as a result of a posttraumatic origin, with hematogenous etiology accounting for 18%.
The long bones of the lower limb, such as the femur and tibia, were involved in 94 cases, whereas the humerus was involved in 6.
The majority of patients (45%) were semi-skilled, followed by 20% skilled, 15% shopkeepers, and so on.
Twelve individuals had diabetes, and 10 had hypertension.
Among walking aids, 35% of the patients were found to be using walking aids such as a crutch or walking stick before the index surgery.
To avoid inter-observer bias, an orthopedic surgeon validated the existence of sequestrum in 65 of 100 patients based on preoperative radiographs. Preoperative MRI was performed on 25 patients at the discretion of the surgeon.
Functional outcome
Lower Extremity Functional Scale functional score
The Lower Extremity Functional Scale consists of a series of 20 questions, each of which is rated on a 5-point ordinal scale ranging from 0 (very difficult/impossible to accomplish) to 4 (no difficulty). The functional capacity was to express nominally and was scored out of a maximum of 80, with a minimal observable change of 9 points regarded clinically significant. The mean preoperative LEFS was 44.1±3.59 (19 to 73).
Musculoskeletal Tumor Society-emotional status
The emotional acceptance level was assessed at the time of presentation following a detailed explanation of the problem and the comprehensive management of the disease involved, including the possibility of recurrence, staged procedures, costs involved, several hospital visits, regular follow-up, and so on.
In our study, 60% of patients disliked their condition at the time of presentation, whereas 36% accepted it. In our study, the emotional aspect of MSTS indicates that none of the cases showed enthusiasm or satisfaction. However, 36% of cases were accepted, and 60% of cases were disliked.
The association for the study and application of the method of Ilizarov criteria functional score
The ASAMI criteria contained 2 components: a radiologically measured bone score and a history and clinical examination-based functional score. The ASAMI functional score was divided into 4 categories as follows: Excellent: active, no limp, minimal stiffness (loss of 15° knee extension/dorsiflexion of ankles), no reflex sympathetic dystrophy, and no pain. Good: active with one or more of the following symptoms: limp, stiffness, Reflex Sympathetic Dystrophy (RSD), or considerable pain. Fair: active, with 3 or more of the following symptoms: limp, stiffness, RSD, and considerable pain. Poor: inactivity (unemployment or inability to do everyday activities due to injury) and amputation.
In our study, preoperative ASAMI was found to be outstanding (4%), fair (62%), good (24%), and bad (10%).
Cierny-Mader classification (Physiological)
Most participants (83%) belong to host A, and 13% belong to host B.
Cierny-Mader classification (Anatomical)
The majority were Cierny-made type IV patient population (42%), 9% were type I, 22% were type II, and 21% patients belonged to Cierny-mader host-A type.
Musculoskeletal Tumor Society-Functional category
There are 22 cases of chronic osteomyelitis with partial impairment, 36 cases with recreational restriction, and 2 cases with no restriction. Among infected non-:union: cases, 2 had entire disability, 15 had recreational restrictions, and 23 had partial impairment.
Culture reports
According to the culture reports, 78% of the samples were culture-positive. Methicillin-sensitive Staphylococcus aureus accounted for 21% of the gram-negative organisms grown, while methicillin-resistant S. aureus accounted for 16% of the samples (Table 1).
Antibiotic treatment
Nine cases out of 19 with hematogenous osteomyelitis had intraoperative culture growth of methicillin-sensitive S. aureus and were given antibiotics for 6 weeks. In the intraoperative cultures of 4 patients, no growth was identified. Cloxacillin was given to 23 patients, Meropenem to 11 individuals, Septran to 8 patients, Linezolid to 8 patients, and Vancomycin to 7 patients. The average length of antibiotic administration was 6 5.06 weeks (95% CI, 4.3-6.4).
Emotional status outcome
After 3 months, there was a decrease in the percentage of patients who disliked their condition (63% to 20%), as well as an increase in the percentage of patients who accepted and understood the problems with their illness and the weight of therapy (33% to 47%). Following surgery, 24% of patients were satisfied after 3 months, and none of the patients were excited at postoperative.
Functional outcome
There was a total of 21 patients with infected non-:union: who returned for a 6-month follow-up. Preoperatively, 7 cases (33.4%) were in the partial disability category, while 5 cases (23.8%) were in the postoperative partial disability category. Recreational limitation was seen in 14 cases (67.6%), whereas the overall number of patients with recreational restriction after surgery was 16 (76.1%). There were no people who were completely disabled or had no limits. According to the MSTS-functional scale, the classification of the 17 patients with infected non-:union: 9th month postop is as follows:
Preoperative vs 9th month postoperative MSTS-functional status in the infected non-:union: group
During the study period, 17 out of 29 patients (5 patients; ≤9months postoperative) were followed up 9th month after the index operation. The number of patients in the partial disability group decreased from 11 to 7, while the number of patients in the recreational limitation group increased from 5 to 10. In addition, 58.5% of patients with infected non-:union: were physically followed up for up to 9th month postop.
6-month postoperative change in ASAMI-functional outcome in patients with infected non-:union: and infected non-:union: group
The number of patients in the poor category decreased from 4 (16.6%) to 1 (4.1%). Preoperatively, there were 17 (70.7%) patients classified as fair, while postoperatively, the number decreased to 12 (50%) individuals. The number of patients classified as good increased from 3 (12.5%) preoperatively to 11 (45.8%) postoperatively. Notably, there was a significant improvement in functional outcomes among patients who progressed from the fair to good category and from the poor to fair category.
Preoperative vs 9th month postoperative functional outcome infected non-:union: group
At 9th month postoperative, the number of patients in the fair group decreased from 12 to 9, whereas the number of patients in the good category increased from 2 to 6.
Preoperative vs 6-month postoperative functional outcome in the chronic osteomyelitis group
There were 7 (33.2%) partially impaired patients preoperatively, while only 5 (22.8%) remained partially disabled postoperatively. At 6 months postoperatively, 2 patients in the partially impaired group who were classified as just recreationally restricted improved.
Preoperative vs 6-month postoperative functional outcome (Based on ASAMI)
Preoperatively, 14 (66.7%) patients were in the fair or poor group; however, the number of patients in this category decreased to 9 (42.8%) after surgery. The number of patients in the good group increased from 6 (28%) prior to surgery to 9 (42.9%) 6 months later, indicating an improvement in their functional status. According to Table 2, the number of patients in the excellent group increased from 1 (4.8%) preoperatively to 3 (14.3%) 6 months later.
Preoperative vs 9th month postop functional outcome (Based on MSTS-functional)
At 9th month postop follow-up, the number of partially disabled patients dropped from 6 (41.7%) preoperatively to 5 (35.72%). Preoperatively, there were 8 (58.3%) patients who had recreational restrictions, and this number decreased to 7 (50%) at the 9th month postop follow-up.
At 9th month follow-up, no restrictions were seen in 2 (14.28%) of cases (Table 3).
Preoperative vs 9th month postoperative functional outcome (MSTS)
According to the functional outcome based on MSTS, 13 patients were classified as poor, fair, and good prior to surgery. Following surgery, the number of patients increased to 7 in the fair category, 5 in the good category, and 2 in the excellent category.
Primary diagnosis vs clinical improvement at 9th month postop
At 9th month postop, 42 patients (64.6%) out of 61 patients with chronic osteomyelitis had substantial functional improvement, while 15 patients (44.1%) with infected non-:union: had significant functional improvement (P = 0.04; Table 4).
There was no substantial clinical improvement in 19 (42.2%) individuals with chronic osteomyelitis. This was related to a number of prognostic factors:
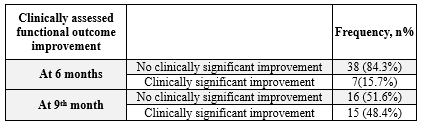
The total number of patients examined at 6 months was 45, with 15.7% showing clinically meaningful improvement in the functional outcome, and the rest showed no improvement (Table 5).
One 9th month after surgery, there were 31 patients with clinical follow-ups, 17 of whom were infected non-:union: patients, and 14 were chronic osteomyelitis patients. According to LEFS, 15 patients (48.6%) showed significant functional improvement, whereas the remaining 16 (51.6%) showed no clinical improvement.
Relapse rates were examined among different patient groups based on criteria such as culture positivity, primary diagnosis, cause of osteomyelitis, and preoperative MRI.
Within 9th month postop follow-up, 20.78% of the 77 patients who were culture positive had recurrence, while 15% of the 20 patients who had no growth on intraoperative cultures had relapse.
There was a decrease in the number of patients who followed up at 6 months post-surgery for chronic osteomyelitis, with a total of 21 patients included in the follow-up. At 6 months post-surgery, 9 patients (24.3%) in the posttraumatic group had recurrence of infection, whereas 1 patient had relapse. At 6 months, the percentage of recurrence in the MRI group was 13.3% (n = 2) and 25% (n = 8) in the non-MRI group (Table 6).
Discussion
Recurrence of chronic osteomyelitis has been observed even after 50 years of symptom-free interval. The recurring pattern of microbiological profiles is poorly known (10). The current study demonstrates a greater rate of infection recurrence or relapse in posttraumatic osteomyelitis. Chronic osteomyelitis relapsed at a rate of 19.8%.
According to the literature, the recurrence rate of chronic osteomyelitis ranged from 0% to 48%. According to Garcia del Pozo et al, 22.4% of people relapse (11).
Uçkay et al suggested that the bone once infected becomes a vulnerable area of bacterial adhesion when transient bacteremia occurs due to any reason whether obvious or not.
Wang et al (12) investigated the use of the induced membrane approach for reconstruction in 424 individuals who had been certified as "cured" of infection. In total, 52 patients suffered a recurrence of infection. Among these, 27.8% had the same bacterium as the initial infection.
In the current investigation, the majority of gram-negative organisms cultivated were methicillin-susceptible S. aureus (21%), with methicillin-resistant S. aureus accounting for 16% of samples. Methicillin-resistant S. aureus was the second most common causal organism of long bone infection, accounting for 16 of 81 positive culture growths, or roughly 20% of all bacterial cultures.
According to Garcia Pozo et al, tibia (62.1%) is the most usually affected bone, and S. aureus (58.5%) is the most prevalent pathogen.
In patients with osteomyelitis, treatment includes radical surgical debridement with or without antibiotic beads/cement spacers, as well as saucerization, sequestrectomy, and sinus tract excision.
The majority of studies advocate 6 weeks of intravenous (IV) antibiotic medication followed by further oral therapy for an unlimited period of time. However, reducing the length of IV antibiotic therapy to 1 week, followed by oral medication, did not result in increased remission rates (13).
Staphylococcus aureus is the most common organism responsible for both acute and chronic bone infections because it creates a biofilm that has the potential to rapidly develop antibiotic resistance and express virulence factors, regardless of the patient's immunological condition.
In our study, the average length of antibiotic administration was 6 weeks. Cloxacillin was the most commonly used antibiotic in 23 cases, Meropenem in 11, Septran in 8, Linezolid in 8, and Vancomycin in 7 cases.
Tice et al observed in their analysis of 454 cases of chronic osteomyelitis treated solely with outpatient-based parenteral therapy that both the initial pathogen and the type of antibiotic used for treatment determined recurrence. Pseudomonas aeruginosa presented a risk that was more than twice as high as that of S. aureus (14).
When necessary, a preoperative MRI may be performed to obtain a full view of bone and soft tissue, as well as to determine the precise extent of disease (15).
Jorge et al examined 192 patients suffering from posttraumatic osteomyelitis. They observed that recurrence was linked to elderly patients, intraoperative blood transfusions, and P. aeruginosa (16).
In our study, 25% of patients got a preoperative MRI, which was entirely at the discretion of the surgeon, taking into account the patient's financial situation, the extent and severity of the condition, and the surgical approach.
In our study, 19.3% of them had a recurrence of infection at any point in time over the 9th month follow-up, and 7.3% required repeat surgery during their hospital stay.
Many factors influenced the functional result following surgery, including mental state, number of previous treatments, degree of bone involvement, therapy decision for limb salvage, patient compliance to treatment, and so on.
In our study, we found a substantial clinical improvement in functional outcome in 7.6% of 91 patients who were followed up on 3 months after surgical debridement and 15.5% of 45 patients who were followed up on 6 months.
When compared to other groups, Cierny-Mader stage-1, hematogenous variety, and culture-negative osteomyelitis were characteristics that reduced the risks of recurrence.
Thirty-one patients were followed upto 9th month; 14 had chronic osteomyelitis, and 17 had infected non-:union:.
Patients with posttraumatic osteomyelitis had a greater recurrence rate (24.3%) than those with hematogenous (primary osteomyelitis; 10%).
Subramanyam et al investigated recurrence risk factors in 147 chronic osteomyelitis patients and found that polymicrobial growth and extended-spectrum beta-lactamase generating Enterobacteriaceae increased the likelihood of chronic osteomyelitis recurrence (17).
According to Petfield et al (18), recurrence is dictated by bone loss, the presence of devascularized bone, and the duration of antibiotic therapy. In a study of 142 cases with posttraumatic osteomyelitis, Chadayammuri et al (19) observed that polymicrobial development and a lack of skin cover were factors in poor prognosis. The administration of parenteral and oral antibiotics in sequence was associated with a lower frequency of ill outcomes.
According to Pozo et al, the length of chronic osteomyelitis for more than 3 months, bone exposure, and the need for further treatments (such as flaps) all contributed to the possibility of recurrence. The average time between debridement and the first signs of relapse was 10 months (2 weeks; 80 months).
The current study had short-term follow-up; therefore, definitive results about infection recurrence and long-term functional outcomes may not be conclusive.
The significance of this work is that it targets an infectious condition that requires early diagnosis at the community level because the burden of disease may interfere with the daily activities of people who belong to the lower-middle class. There is little data on relapse rates and functional outcomes following surgery in chronic osteomyelitis; therefore, this study can shed light on these facets of the disease.
Conclusion
This study demonstrates a higher rate of infection recurrence or relapse in posttraumatic osteomyelitis. Chronic osteomyelitis relapsed at a rate of 19.8%. At 6 months, the functional outcome findings were better. Disease burden, financial issues, disability, and long duration of therapy all have an impact on the patient's mental state, which may further impact treatment adherence.
Acknowledgement
None.
Funding sources
The authors received no financial support for this article's research, authorship, or publication.
Ethical statement
The study was performed per the Declaration of Helsinki, and written informed consent was obtained from the study participants. Institutional ethical approval (EC/23/01) was obtained for the study protocol.
Conflicts of interest
The authors declare no conflict of interest in this research.
Author contributions
DV and AT analyzed and interpreted the osteomyelitis patient’s clinical and microbiological data. MS performed the surgical interventions and was a major contributor to writing the manuscript. KM supervised the total work and edited the manuscript. All authors read and approved the final manuscript.
The relapse is defined as the recurrence of infection in the same location where it was previously thought to be cleared and was particularly treated with surgery.
Statistical analysis
Demographic, clinical, and laboratory characteristics were all documented in a proforma. An analysis of variance (ANOVA) was performed to analyze continuous variables with preoperative frequency data. Chi-square tests were used to examine categorical variables that had a functional consequence. Non-categorical results were compared using a Student’s t-test. The relationship between the score and clinical profile was assessed using Pearson correlation analysis. P values less than 0.05 were considered statistically significant. Statistical analysis was done using SPSS version 22.0.
Results
Among the 100 patients, 60 had chronic osteomyelitis, and 40 had infected non-:union:. The average age was 35 years. Males made up 82% of the patients.
The majority of patients (82%) were diagnosed with chronic osteomyelitis as a result of a posttraumatic origin, with hematogenous etiology accounting for 18%.
The long bones of the lower limb, such as the femur and tibia, were involved in 94 cases, whereas the humerus was involved in 6.
The majority of patients (45%) were semi-skilled, followed by 20% skilled, 15% shopkeepers, and so on.
Twelve individuals had diabetes, and 10 had hypertension.
Among walking aids, 35% of the patients were found to be using walking aids such as a crutch or walking stick before the index surgery.
To avoid inter-observer bias, an orthopedic surgeon validated the existence of sequestrum in 65 of 100 patients based on preoperative radiographs. Preoperative MRI was performed on 25 patients at the discretion of the surgeon.
Functional outcome
Lower Extremity Functional Scale functional score
The Lower Extremity Functional Scale consists of a series of 20 questions, each of which is rated on a 5-point ordinal scale ranging from 0 (very difficult/impossible to accomplish) to 4 (no difficulty). The functional capacity was to express nominally and was scored out of a maximum of 80, with a minimal observable change of 9 points regarded clinically significant. The mean preoperative LEFS was 44.1±3.59 (19 to 73).
Musculoskeletal Tumor Society-emotional status
The emotional acceptance level was assessed at the time of presentation following a detailed explanation of the problem and the comprehensive management of the disease involved, including the possibility of recurrence, staged procedures, costs involved, several hospital visits, regular follow-up, and so on.
In our study, 60% of patients disliked their condition at the time of presentation, whereas 36% accepted it. In our study, the emotional aspect of MSTS indicates that none of the cases showed enthusiasm or satisfaction. However, 36% of cases were accepted, and 60% of cases were disliked.
The association for the study and application of the method of Ilizarov criteria functional score
The ASAMI criteria contained 2 components: a radiologically measured bone score and a history and clinical examination-based functional score. The ASAMI functional score was divided into 4 categories as follows: Excellent: active, no limp, minimal stiffness (loss of 15° knee extension/dorsiflexion of ankles), no reflex sympathetic dystrophy, and no pain. Good: active with one or more of the following symptoms: limp, stiffness, Reflex Sympathetic Dystrophy (RSD), or considerable pain. Fair: active, with 3 or more of the following symptoms: limp, stiffness, RSD, and considerable pain. Poor: inactivity (unemployment or inability to do everyday activities due to injury) and amputation.
In our study, preoperative ASAMI was found to be outstanding (4%), fair (62%), good (24%), and bad (10%).
Cierny-Mader classification (Physiological)
Most participants (83%) belong to host A, and 13% belong to host B.
Cierny-Mader classification (Anatomical)
The majority were Cierny-made type IV patient population (42%), 9% were type I, 22% were type II, and 21% patients belonged to Cierny-mader host-A type.
Musculoskeletal Tumor Society-Functional category
There are 22 cases of chronic osteomyelitis with partial impairment, 36 cases with recreational restriction, and 2 cases with no restriction. Among infected non-:union: cases, 2 had entire disability, 15 had recreational restrictions, and 23 had partial impairment.
Culture reports
According to the culture reports, 78% of the samples were culture-positive. Methicillin-sensitive Staphylococcus aureus accounted for 21% of the gram-negative organisms grown, while methicillin-resistant S. aureus accounted for 16% of the samples (Table 1).
Table 1. The culture report of study samples |
Nine cases out of 19 with hematogenous osteomyelitis had intraoperative culture growth of methicillin-sensitive S. aureus and were given antibiotics for 6 weeks. In the intraoperative cultures of 4 patients, no growth was identified. Cloxacillin was given to 23 patients, Meropenem to 11 individuals, Septran to 8 patients, Linezolid to 8 patients, and Vancomycin to 7 patients. The average length of antibiotic administration was 6 5.06 weeks (95% CI, 4.3-6.4).
Emotional status outcome
After 3 months, there was a decrease in the percentage of patients who disliked their condition (63% to 20%), as well as an increase in the percentage of patients who accepted and understood the problems with their illness and the weight of therapy (33% to 47%). Following surgery, 24% of patients were satisfied after 3 months, and none of the patients were excited at postoperative.
Functional outcome
There was a total of 21 patients with infected non-:union: who returned for a 6-month follow-up. Preoperatively, 7 cases (33.4%) were in the partial disability category, while 5 cases (23.8%) were in the postoperative partial disability category. Recreational limitation was seen in 14 cases (67.6%), whereas the overall number of patients with recreational restriction after surgery was 16 (76.1%). There were no people who were completely disabled or had no limits. According to the MSTS-functional scale, the classification of the 17 patients with infected non-:union: 9th month postop is as follows:
Preoperative vs 9th month postoperative MSTS-functional status in the infected non-:union: group
During the study period, 17 out of 29 patients (5 patients; ≤9months postoperative) were followed up 9th month after the index operation. The number of patients in the partial disability group decreased from 11 to 7, while the number of patients in the recreational limitation group increased from 5 to 10. In addition, 58.5% of patients with infected non-:union: were physically followed up for up to 9th month postop.
6-month postoperative change in ASAMI-functional outcome in patients with infected non-:union: and infected non-:union: group
The number of patients in the poor category decreased from 4 (16.6%) to 1 (4.1%). Preoperatively, there were 17 (70.7%) patients classified as fair, while postoperatively, the number decreased to 12 (50%) individuals. The number of patients classified as good increased from 3 (12.5%) preoperatively to 11 (45.8%) postoperatively. Notably, there was a significant improvement in functional outcomes among patients who progressed from the fair to good category and from the poor to fair category.
Preoperative vs 9th month postoperative functional outcome infected non-:union: group
At 9th month postoperative, the number of patients in the fair group decreased from 12 to 9, whereas the number of patients in the good category increased from 2 to 6.
Preoperative vs 6-month postoperative functional outcome in the chronic osteomyelitis group
There were 7 (33.2%) partially impaired patients preoperatively, while only 5 (22.8%) remained partially disabled postoperatively. At 6 months postoperatively, 2 patients in the partially impaired group who were classified as just recreationally restricted improved.
Preoperative vs 6-month postoperative functional outcome (Based on ASAMI)
Preoperatively, 14 (66.7%) patients were in the fair or poor group; however, the number of patients in this category decreased to 9 (42.8%) after surgery. The number of patients in the good group increased from 6 (28%) prior to surgery to 9 (42.9%) 6 months later, indicating an improvement in their functional status. According to Table 2, the number of patients in the excellent group increased from 1 (4.8%) preoperatively to 3 (14.3%) 6 months later.
Table 2. Preoperative vs 6-month postoperative functional outcome |
At 9th month postop follow-up, the number of partially disabled patients dropped from 6 (41.7%) preoperatively to 5 (35.72%). Preoperatively, there were 8 (58.3%) patients who had recreational restrictions, and this number decreased to 7 (50%) at the 9th month postop follow-up.
At 9th month follow-up, no restrictions were seen in 2 (14.28%) of cases (Table 3).
|
Table 3. Preoperative vs 9th month postop MSTS-functional outcome (n=14)
 |
According to the functional outcome based on MSTS, 13 patients were classified as poor, fair, and good prior to surgery. Following surgery, the number of patients increased to 7 in the fair category, 5 in the good category, and 2 in the excellent category.
Primary diagnosis vs clinical improvement at 9th month postop
At 9th month postop, 42 patients (64.6%) out of 61 patients with chronic osteomyelitis had substantial functional improvement, while 15 patients (44.1%) with infected non-:union: had significant functional improvement (P = 0.04; Table 4).
There was no substantial clinical improvement in 19 (42.2%) individuals with chronic osteomyelitis. This was related to a number of prognostic factors:
- Four patients underwent a primary flap procedure, after which they were immobilized for longer periods of time to minimize soft tissue issues that could harm the limb.
- Seven patients had had more than 3 previous surgeries, either at our institute or elsewhere.
- In intraoperative cultures, 5 individuals exhibited resistant Pseudomonas aeruginosa.
Table 4. Association between diagnosis and clinical improvement at 9th month (LEFS) |
One 9th month after surgery, there were 31 patients with clinical follow-ups, 17 of whom were infected non-:union: patients, and 14 were chronic osteomyelitis patients. According to LEFS, 15 patients (48.6%) showed significant functional improvement, whereas the remaining 16 (51.6%) showed no clinical improvement.
|
Table 5. Functional outcome at 6 months and 9th month postop (LEFS)
 |
Within 9th month postop follow-up, 20.78% of the 77 patients who were culture positive had recurrence, while 15% of the 20 patients who had no growth on intraoperative cultures had relapse.
There was a decrease in the number of patients who followed up at 6 months post-surgery for chronic osteomyelitis, with a total of 21 patients included in the follow-up. At 6 months post-surgery, 9 patients (24.3%) in the posttraumatic group had recurrence of infection, whereas 1 patient had relapse. At 6 months, the percentage of recurrence in the MRI group was 13.3% (n = 2) and 25% (n = 8) in the non-MRI group (Table 6).
Table 6. Association between culture positivity and relapse; primary diagnosis and relapse; preoperative MRI and relapse at 6 months |
Recurrence of chronic osteomyelitis has been observed even after 50 years of symptom-free interval. The recurring pattern of microbiological profiles is poorly known (10). The current study demonstrates a greater rate of infection recurrence or relapse in posttraumatic osteomyelitis. Chronic osteomyelitis relapsed at a rate of 19.8%.
According to the literature, the recurrence rate of chronic osteomyelitis ranged from 0% to 48%. According to Garcia del Pozo et al, 22.4% of people relapse (11).
Uçkay et al suggested that the bone once infected becomes a vulnerable area of bacterial adhesion when transient bacteremia occurs due to any reason whether obvious or not.
Wang et al (12) investigated the use of the induced membrane approach for reconstruction in 424 individuals who had been certified as "cured" of infection. In total, 52 patients suffered a recurrence of infection. Among these, 27.8% had the same bacterium as the initial infection.
In the current investigation, the majority of gram-negative organisms cultivated were methicillin-susceptible S. aureus (21%), with methicillin-resistant S. aureus accounting for 16% of samples. Methicillin-resistant S. aureus was the second most common causal organism of long bone infection, accounting for 16 of 81 positive culture growths, or roughly 20% of all bacterial cultures.
According to Garcia Pozo et al, tibia (62.1%) is the most usually affected bone, and S. aureus (58.5%) is the most prevalent pathogen.
In patients with osteomyelitis, treatment includes radical surgical debridement with or without antibiotic beads/cement spacers, as well as saucerization, sequestrectomy, and sinus tract excision.
The majority of studies advocate 6 weeks of intravenous (IV) antibiotic medication followed by further oral therapy for an unlimited period of time. However, reducing the length of IV antibiotic therapy to 1 week, followed by oral medication, did not result in increased remission rates (13).
Staphylococcus aureus is the most common organism responsible for both acute and chronic bone infections because it creates a biofilm that has the potential to rapidly develop antibiotic resistance and express virulence factors, regardless of the patient's immunological condition.
In our study, the average length of antibiotic administration was 6 weeks. Cloxacillin was the most commonly used antibiotic in 23 cases, Meropenem in 11, Septran in 8, Linezolid in 8, and Vancomycin in 7 cases.
Tice et al observed in their analysis of 454 cases of chronic osteomyelitis treated solely with outpatient-based parenteral therapy that both the initial pathogen and the type of antibiotic used for treatment determined recurrence. Pseudomonas aeruginosa presented a risk that was more than twice as high as that of S. aureus (14).
When necessary, a preoperative MRI may be performed to obtain a full view of bone and soft tissue, as well as to determine the precise extent of disease (15).
Jorge et al examined 192 patients suffering from posttraumatic osteomyelitis. They observed that recurrence was linked to elderly patients, intraoperative blood transfusions, and P. aeruginosa (16).
In our study, 25% of patients got a preoperative MRI, which was entirely at the discretion of the surgeon, taking into account the patient's financial situation, the extent and severity of the condition, and the surgical approach.
In our study, 19.3% of them had a recurrence of infection at any point in time over the 9th month follow-up, and 7.3% required repeat surgery during their hospital stay.
Many factors influenced the functional result following surgery, including mental state, number of previous treatments, degree of bone involvement, therapy decision for limb salvage, patient compliance to treatment, and so on.
In our study, we found a substantial clinical improvement in functional outcome in 7.6% of 91 patients who were followed up on 3 months after surgical debridement and 15.5% of 45 patients who were followed up on 6 months.
When compared to other groups, Cierny-Mader stage-1, hematogenous variety, and culture-negative osteomyelitis were characteristics that reduced the risks of recurrence.
Thirty-one patients were followed upto 9th month; 14 had chronic osteomyelitis, and 17 had infected non-:union:.
Patients with posttraumatic osteomyelitis had a greater recurrence rate (24.3%) than those with hematogenous (primary osteomyelitis; 10%).
Subramanyam et al investigated recurrence risk factors in 147 chronic osteomyelitis patients and found that polymicrobial growth and extended-spectrum beta-lactamase generating Enterobacteriaceae increased the likelihood of chronic osteomyelitis recurrence (17).
According to Petfield et al (18), recurrence is dictated by bone loss, the presence of devascularized bone, and the duration of antibiotic therapy. In a study of 142 cases with posttraumatic osteomyelitis, Chadayammuri et al (19) observed that polymicrobial development and a lack of skin cover were factors in poor prognosis. The administration of parenteral and oral antibiotics in sequence was associated with a lower frequency of ill outcomes.
According to Pozo et al, the length of chronic osteomyelitis for more than 3 months, bone exposure, and the need for further treatments (such as flaps) all contributed to the possibility of recurrence. The average time between debridement and the first signs of relapse was 10 months (2 weeks; 80 months).
The current study had short-term follow-up; therefore, definitive results about infection recurrence and long-term functional outcomes may not be conclusive.
The significance of this work is that it targets an infectious condition that requires early diagnosis at the community level because the burden of disease may interfere with the daily activities of people who belong to the lower-middle class. There is little data on relapse rates and functional outcomes following surgery in chronic osteomyelitis; therefore, this study can shed light on these facets of the disease.
Conclusion
This study demonstrates a higher rate of infection recurrence or relapse in posttraumatic osteomyelitis. Chronic osteomyelitis relapsed at a rate of 19.8%. At 6 months, the functional outcome findings were better. Disease burden, financial issues, disability, and long duration of therapy all have an impact on the patient's mental state, which may further impact treatment adherence.
Acknowledgement
None.
Funding sources
The authors received no financial support for this article's research, authorship, or publication.
Ethical statement
The study was performed per the Declaration of Helsinki, and written informed consent was obtained from the study participants. Institutional ethical approval (EC/23/01) was obtained for the study protocol.
Conflicts of interest
The authors declare no conflict of interest in this research.
Author contributions
DV and AT analyzed and interpreted the osteomyelitis patient’s clinical and microbiological data. MS performed the surgical interventions and was a major contributor to writing the manuscript. KM supervised the total work and edited the manuscript. All authors read and approved the final manuscript.
References
1. Uçkay I, Assal M, Legout L, Rohner P, Stern R, Lew D, et al. Recurrent osteomyelitis caused by infection with different bacterial strains without obvious source of reinfection. J Clin Microbiol. 2006;44(3):1194-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Wu Z, Zeng D, Yao J, Bian Y, Gu Y, Meng Z, et al. Research progress on diagnosis and treatment of chronic osteomyelitis. J Chin Med Sci. 2019;34(3):211-20. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Masrouha KZ, Raad ME, Saghieh SS. A novel treatment approach to infected non:union: of long bones without systemic antibiotics. Strategies Trauma Limb Reconstr. 2018;13(1):13-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Lowenberg DW, DeBaun M, Suh GA. Newer perspectives in the treatment of chronic osteomyelitis: A preliminary outcome report. Injury. 2019;50(1):S56-61. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Geraghty T, Laporta G. Current health and economic burden of chronic diabetic osteomyelitis. Expert Rev Pharmacoecon Outcomes Res. 2019;19(3):279-86. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Ellur V, Kumar G, Sampath JS. Treatment of chronic hematogenous osteomyelitis in children with antibiotic impregnated calcium sulphate. J Pediatr Orthop. 2021;41(2):127-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Bose D, Kugan R, Stubbs D, McNally M. Management of infected non:union: of the long bones by a multidisciplinary team. Bone Joint J. 2015;97(6):814-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Biruk WL, Wubshet K. Chronic Osteomyelitis at Tikur Anbessa Hospital, Addis Ababa University, Ethiopia. East Cent Afr J. 2007;12:33-41. [View at Publisher] [Google Scholar]
9. Chrousos GP. Stress, chronic inflammation, and emotional and physical well-being: concurrent effects and chronic sequelae. J Allergy Clin Immunol. 2000;106(5):S275-91. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Uçkay I, Jugun K, Gamulin A, Wagener J, Hoffmeyer P, Lew D. Chronic osteomyelitis. Curr Infect Dis Rep. 2012;14:566-75. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Garcia del Pozo E, Collazos J, Carton JA, Camporro D, Asensi V. Factors predictive of relapse in adult bacterial osteomyelitis of long bones. BMC Infect Dis. 2018;18(1):635. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Wang X, Wang S, Fu J, Sun D, Shen J, Xie Z. Risk factors associated with recurrence of extremity osteomyelitis treated with the induced membrane technique. Injury. 2020;51(2):307-11. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Okumura N, Hayakawa K, Yamamoto K, Yamada G, Mezaki K, Ohmagari N. Effectiveness of oral cephalexin in antibiotic-course completion for methicillin-susceptible Staphylococcus aureus-induced bacteremic vertebral osteomyelitis. BMC Infect Dis. 2023;23(1):307. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Tice AD, Hoaglund PA, Shoultz DA. Risk factors and treatment outcomes in osteomyelitis. J Antimicrob Chemother. 2003;51(5):1261-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Marais LC, Ferreira N, Aldous C, Le Roux TL. The management of chronic osteomyelitis: Part I-Diagnostic work-up and surgical principles. SA Orthopaedic Journal. 2014;13(2):42-8. [View at Publisher] [Google Scholar]
16. Jorge LS, Chueire AG, Fucuta PS, Machado MN, Oliveira MG, Nakazone MA, et al. Predisposing factors for recurrence of chronic posttraumatic osteomyelitis: a retrospective observational cohort study from a tertiary referral center in Brazil. Patient Saf Surg. 2017;11:17. [] [DOI] [PMID] [Google Scholar]
17. Subramanyam KN, Mundargi AV, Prabhu MV, Gopakumar KU, Gowda DA, Reddy DR. Surgical management of chronic osteomyelitis: Organisms, recurrence and treatment outcome. Chinese. Chin J Traumatol. 2023;26(4):228-35. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Petfield JL, Tribble DR, Potter BK, Lewandowski LR, Weintrob AC, Krauss M, et al. Is bone loss or devascularization associated with recurrence of osteomyelitis in wartime open tibia fractures?. Clin Orthop Relat Res. 2019;477(4):789-801. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Chadayammuri V, Herbert B, Hao J, Mavrogenis A, Quispe JC, Kim JW, et al. Factors associated with adverse postoperative outcomes in patients with long bone post-traumatic osteomyelitis. Eur J Orthop Surg Traumatol. 2017;27(7):877–882. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).




