Volume 7, Issue 4 (Journal of Clinical and Basic Research (JCBR) 2023)
jcbr 2023, 7(4): 20-22 |
Back to browse issues page
Ethics code: GMC/IEC-20/02-01
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dias M C, kudalkar U, Madhale N, Kavlekar A K. Variations in the drainage pattern of the hepatic veins into the inferior vena cava: A cadaveric study. jcbr 2023; 7 (4) :20-22
URL: http://jcbr.goums.ac.ir/article-1-421-en.html
URL: http://jcbr.goums.ac.ir/article-1-421-en.html
1- Department of Anatomy, Goa Medical College, Bambolim, Goa, India , diasmerle@gmail.com
2- Department of Anatomy, Goa Medical College, Bambolim, Goa, India
2- Department of Anatomy, Goa Medical College, Bambolim, Goa, India
Full-Text [PDF 490 kb]
(93 Downloads)
| Abstract (HTML) (330 Views)
Full-Text: (46 Views)
Introduction
Hepatic veins are considered to be a communication between the portal and systemic venous vasculature. These veins traverse the substance of the liver, draining different segments of the liver and ultimately emptying into the floor of the inferior vena cava (IVC).
There are 3 main channels of hepatic veins, namely right, middle, and left hepatic veins. Lying in the sagittal plane is the middle hepatic vein and is thus considered an important landmark in the field of radiology (1). The liver also has minor hepatic venous vasculature, which is smaller in diameter than the major veins.
The hepatic venous outflow is an important aspect of the functioning of liver homeostasis. Hepatic venous obstruction can lead to various degrees of hepatic dysfunction or failure. It is one of the major causes of portal venous hypertension.
In cirrhotic patients, patients with obstructive jaundice or those undergoing liver transplantation, there may be occlusion to the hepatic venous outflow, which can have a tremendous effect on the patient outcome (2). Thus, a detailed understanding of the anatomical structure of hepatic venous vasculature with regard to the IVC is of great importance to surgeons for procedures involving the liver, such as liver transplantation, hepatic trauma, and hepatic resection. In this study, we observed variations in the number, along with the pattern of openings of the hepatic venous vasculature into the retro hepatic part of the IVC.
Methods
This research involved a comprehensive gross examination of the numerical and pattern variations in the outflow of the hepatic venous vasculature into the inferior vena cava (IVC). Prior to conducting the study, approval was obtained from the Institutional Ethics Committee (code: GMC/IEC-20/02-01; dated 07/02/2020). The total number of livers studied was 84; they were available in the Department of Anatomy, Goa Medical College, Goa. The livers were formalin-fixed livers obtained from donated cadavers used for MBBS dissection classes. Out of 84 livers examined, 9 livers were excluded.
The exclusion criteria were as follows:
1. Stripped off the hepatic part of the IVC.
2. Micronodular or macronodular cirrhosis of the liver; it can change the diameter of the openings of the hepatic veins into the IVC.
The posterior wall of the hepatic part of the IVC was incised to examine the number and patterns of major and minor hepatic venous vasculature outflow channels in the floor of the IVC. Openings with a diameter 1 cm were considered major hepatic veins, whereas the ones with a diameter between 0.5 and 1 cm were considered minor hepatic veins. The openings < 0.5 cm were not considered in this study. An observation was made regarding the occurrence of a single trunk for the left and middle hepatic veins. Measurements were taken using a scale, and the values were noted in an Excel sheet. The pictures of the livers with variations in the number and pattern were recorded and documented.
Results
Numerical Variations
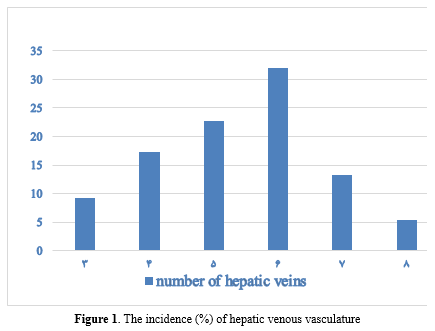
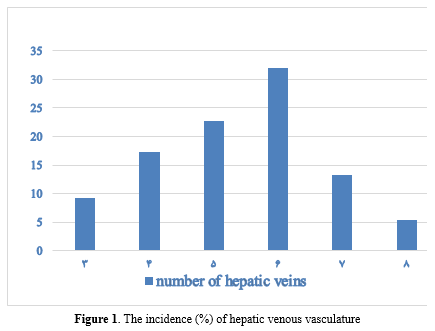
In this research, all the livers examined were drained by both major and minor hepatic venous vasculature. In total, the number of openings of hepatic venous vasculature in IVC ranged from 3 to 8 (Table 1; Figure1). Seven livers with only 3 openings had an incidence of 9.3%, whereas 4 livers with an incidence of 5.3% had 8 openings. The majority of the livers (n = 24; 32%) had 6 openings (Table 1).
The combined number of major hepatic venous vasculature varied from 1 to 4 (Table 2). In 60% of the total number of livers examined, there were 3 major hepatic venous openings, followed by 2 major openings seen in 20 livers with an incidence of 26.7%. Six livers had only 1 major opening, with an incidence of 8% (Table 2).
Pattern Variations
Considering the pattern of the outflow channel of the hepatic venous vasculature in the IVC (Table 3), the majority of the specimens (n = 25) showed a double opening pattern with 1 separate opening for the right side major hepatic vein and a single channel for the middle and left hepatic veins. Twenty-one livers showed a single opening pattern with a separate opening for the right, middle, and left hepatic veins. Three livers showed a triple opening pattern, having a single lumen for the right hepatic vein and 3 lumens draining into a single trunk for the left and middle hepatic veins (Figure 2).

Only 1 liver had a double opening for left and middle major veins into a single trunk with an absent right major hepatic vein.
Fourteen livers had a separate lumen for each of the left and right hepatic veins, and the middle hepatic vein was not present (Figure 3). Twenty-one livers had separate openings for the right, left, and middle hepatic veins (Figure 4).


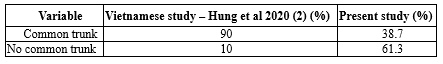
Out of the 75 livers examined, 29 livers had a single trunk for middle and left hepatic veins with 38.7% incidence (Table 4; Figure5).

Discussion
Hepatic venous channels link the portal and systemic circulation. They are formed in the liver parenchyma and terminate by opening into the floor of the IVC. In our study, these veins were divided into major (> 1 cm) and minor (0.5 to 1 cm) hepatic veins, depending upon the diameter of their opening into the floor of the IVC.
The major right hepatic vein (known as the vena hepatica dextra) lies between the posterior and anterior sectors of the right liver lobe; then, it drains superior areas of the anterior sector and posterior sectors of the right liver lobe (3). This one is the largest hepatic vein. In the current study, the incidence of the major right hepatic vein was 97.3% (Table 4).
The major left vein (known as the vena hepatica sinistra) drains lateral sectors, along with the superior part of the medial sectors (3)(4). This was seen in 65 livers with incidence of 86.6% (Table 4).
The major middle hepatic vein (also known as the vena hepatica media) lies between the right and left anatomical lobes of the liver and drains the inferior aspect of the right anterior sectors, along with the inferior aspect of the medial sectors (4). This was seen in 55 livers with an incidence of 73.3% (Table 4).
Accessory hepatic venous vasculature also drains into the lower aspect of the floor of the IVC (8). These were not included in our study.
In Fersia et al ’s study (2010) (7), the incidence of occurrence of all 3 major veins of the liver was 50% compared to an incidence of 66.6% observed in our study.
Considering the pattern of the outflow of the veins into the IVC, there were a total of 29 livers (incidence = 38.6%) with a single major right hepatic vein with a united trunk for the left and middle major veins of the liver. This is comparable to Chi-Hua Fang et al, in which the incidence was 61% (9).
In Hung et al ’s study, the incidence of the presence of a single trunk for the left with middle hepatic vein was 90% (2), compared to the 38.7% incidence found in our study (Table 5).
The awareness of anatomical variations of the drainage pattern of hepatic venous vasculature into the floor of the IVC is essential for physicians and surgeons to understand any pathophysiology in relation to hepatic vein outflow obstruction. This helps in deciding treatment modalities for portal hypertension and thus improving outcomes.
The knowledge of anatomical variations of hepatic veins is highly beneficial to liver transplant surgeons to understand the reconstruction technique that needs to be used to create a new orifice to anastomose combined diameter of left and middle donor hepatic venous vasculature to the recipient's IVC. The occurrence of a single trunk for left and middle hepatic veins is of utmost importance when performing a liver transplant. According to Camargo et al (1996), the incidence of the common trunk is about 62% to 97% (5). In the study by H. V. Duong et al (2019), the technique that was studied to create a new opening was the sectioning of the middle and left hepatic veins before the confluence so that its diameter matches the diameter of the recipient's IVC (2). According to Meunier et al (1993), a technique known as “piggy-back” method, could be used, in which the retro-hepatic segment IVC is joined to the common trunk of the receiver. The advantage of this technique is that it avoids the need for dissection or manipulation of the recipient's IVC. This can help to reduce blood loss, in turn maintaining hemodynamics (6). According to Zhitao Chen et al, the piggyback procedure prevents the chance of possibility of postoperative renal impairment following liver transplantation (10). Belghiti et al (1992) documented and developed the modified piggy-back procedure, which consisted of cavocaval anastomosis done side-to-side on the anterior aspect of the receiver’s right major hepatic vein, thereby reducing outflow obstruction (11).
Conclusion
The liver venous vasculature does show numerous variations in its draining pattern into the retro-hepatic segment of IVC. This knowledge plays a significant role in understanding the severity of hepatic venous outflow obstruction, as it depends on the number of obstructed hepatic veins (8). It is also imperative to evaluate the morphology of the venous drainage prior to any hepatic surgeries, especially in the transplantation of the liver, to prevent the massacre of life-threatening hemorrhage, thus improving postoperative outcomes.
Acknowledgement
I would like to thank my colleagues for their unending support while working on this research topic. The researchers truly acknowledge the precious souls who donated bodies to medicine to aid in research in the field of anatomy. Inferences from this study will enhance the surgeon's overall knowledge, thereby improving patient care. Therefore, the donors, with their kin, deserve our highest appreciation.
Funding sources
The authors did not receive any funding to conduct this study.
Ethical statement
The permission to conduct this study was granted by the Institutional Ethics Committee of Goa Medical College (code: GMC/IEC-20/02-01; dated 03/02/2023).
Conflicts of interest
There are no conflicts of interest between the authors.
Author contributions
Hepatic veins are considered to be a communication between the portal and systemic venous vasculature. These veins traverse the substance of the liver, draining different segments of the liver and ultimately emptying into the floor of the inferior vena cava (IVC).
There are 3 main channels of hepatic veins, namely right, middle, and left hepatic veins. Lying in the sagittal plane is the middle hepatic vein and is thus considered an important landmark in the field of radiology (1). The liver also has minor hepatic venous vasculature, which is smaller in diameter than the major veins.
The hepatic venous outflow is an important aspect of the functioning of liver homeostasis. Hepatic venous obstruction can lead to various degrees of hepatic dysfunction or failure. It is one of the major causes of portal venous hypertension.
In cirrhotic patients, patients with obstructive jaundice or those undergoing liver transplantation, there may be occlusion to the hepatic venous outflow, which can have a tremendous effect on the patient outcome (2). Thus, a detailed understanding of the anatomical structure of hepatic venous vasculature with regard to the IVC is of great importance to surgeons for procedures involving the liver, such as liver transplantation, hepatic trauma, and hepatic resection. In this study, we observed variations in the number, along with the pattern of openings of the hepatic venous vasculature into the retro hepatic part of the IVC.
Methods
This research involved a comprehensive gross examination of the numerical and pattern variations in the outflow of the hepatic venous vasculature into the inferior vena cava (IVC). Prior to conducting the study, approval was obtained from the Institutional Ethics Committee (code: GMC/IEC-20/02-01; dated 07/02/2020). The total number of livers studied was 84; they were available in the Department of Anatomy, Goa Medical College, Goa. The livers were formalin-fixed livers obtained from donated cadavers used for MBBS dissection classes. Out of 84 livers examined, 9 livers were excluded.
The exclusion criteria were as follows:
1. Stripped off the hepatic part of the IVC.
2. Micronodular or macronodular cirrhosis of the liver; it can change the diameter of the openings of the hepatic veins into the IVC.
The posterior wall of the hepatic part of the IVC was incised to examine the number and patterns of major and minor hepatic venous vasculature outflow channels in the floor of the IVC. Openings with a diameter 1 cm were considered major hepatic veins, whereas the ones with a diameter between 0.5 and 1 cm were considered minor hepatic veins. The openings < 0.5 cm were not considered in this study. An observation was made regarding the occurrence of a single trunk for the left and middle hepatic veins. Measurements were taken using a scale, and the values were noted in an Excel sheet. The pictures of the livers with variations in the number and pattern were recorded and documented.
Results
Numerical Variations
In this research, all the livers examined were drained by both major and minor hepatic venous vasculature. In total, the number of openings of hepatic venous vasculature in IVC ranged from 3 to 8 (Table 1; Figure1). Seven livers with only 3 openings had an incidence of 9.3%, whereas 4 livers with an incidence of 5.3% had 8 openings. The majority of the livers (n = 24; 32%) had 6 openings (Table 1).
The combined number of major hepatic venous vasculature varied from 1 to 4 (Table 2). In 60% of the total number of livers examined, there were 3 major hepatic venous openings, followed by 2 major openings seen in 20 livers with an incidence of 26.7%. Six livers had only 1 major opening, with an incidence of 8% (Table 2).
|
Table 1. The number of hepatic veins with incidence
 |
|
Table 2. The incidence of major hepatic veins
 |
Considering the pattern of the outflow channel of the hepatic venous vasculature in the IVC (Table 3), the majority of the specimens (n = 25) showed a double opening pattern with 1 separate opening for the right side major hepatic vein and a single channel for the middle and left hepatic veins. Twenty-one livers showed a single opening pattern with a separate opening for the right, middle, and left hepatic veins. Three livers showed a triple opening pattern, having a single lumen for the right hepatic vein and 3 lumens draining into a single trunk for the left and middle hepatic veins (Figure 2).

Only 1 liver had a double opening for left and middle major veins into a single trunk with an absent right major hepatic vein.
Fourteen livers had a separate lumen for each of the left and right hepatic veins, and the middle hepatic vein was not present (Figure 3). Twenty-one livers had separate openings for the right, left, and middle hepatic veins (Figure 4).


Out of the 75 livers examined, 29 livers had a single trunk for middle and left hepatic veins with 38.7% incidence (Table 4; Figure5).
|
Table 4. The incidence of occurrence of middle, left, and right major hepatic veins
 |

Discussion
Hepatic venous channels link the portal and systemic circulation. They are formed in the liver parenchyma and terminate by opening into the floor of the IVC. In our study, these veins were divided into major (> 1 cm) and minor (0.5 to 1 cm) hepatic veins, depending upon the diameter of their opening into the floor of the IVC.
The major right hepatic vein (known as the vena hepatica dextra) lies between the posterior and anterior sectors of the right liver lobe; then, it drains superior areas of the anterior sector and posterior sectors of the right liver lobe (3). This one is the largest hepatic vein. In the current study, the incidence of the major right hepatic vein was 97.3% (Table 4).
The major left vein (known as the vena hepatica sinistra) drains lateral sectors, along with the superior part of the medial sectors (3)(4). This was seen in 65 livers with incidence of 86.6% (Table 4).
The major middle hepatic vein (also known as the vena hepatica media) lies between the right and left anatomical lobes of the liver and drains the inferior aspect of the right anterior sectors, along with the inferior aspect of the medial sectors (4). This was seen in 55 livers with an incidence of 73.3% (Table 4).
Accessory hepatic venous vasculature also drains into the lower aspect of the floor of the IVC (8). These were not included in our study.
In Fersia et al ’s study (2010) (7), the incidence of occurrence of all 3 major veins of the liver was 50% compared to an incidence of 66.6% observed in our study.
Considering the pattern of the outflow of the veins into the IVC, there were a total of 29 livers (incidence = 38.6%) with a single major right hepatic vein with a united trunk for the left and middle major veins of the liver. This is comparable to Chi-Hua Fang et al, in which the incidence was 61% (9).
In Hung et al ’s study, the incidence of the presence of a single trunk for the left with middle hepatic vein was 90% (2), compared to the 38.7% incidence found in our study (Table 5).
|
Table 5. The incidence of single trunk for left with middle hepatic veins
 |
The knowledge of anatomical variations of hepatic veins is highly beneficial to liver transplant surgeons to understand the reconstruction technique that needs to be used to create a new orifice to anastomose combined diameter of left and middle donor hepatic venous vasculature to the recipient's IVC. The occurrence of a single trunk for left and middle hepatic veins is of utmost importance when performing a liver transplant. According to Camargo et al (1996), the incidence of the common trunk is about 62% to 97% (5). In the study by H. V. Duong et al (2019), the technique that was studied to create a new opening was the sectioning of the middle and left hepatic veins before the confluence so that its diameter matches the diameter of the recipient's IVC (2). According to Meunier et al (1993), a technique known as “piggy-back” method, could be used, in which the retro-hepatic segment IVC is joined to the common trunk of the receiver. The advantage of this technique is that it avoids the need for dissection or manipulation of the recipient's IVC. This can help to reduce blood loss, in turn maintaining hemodynamics (6). According to Zhitao Chen et al, the piggyback procedure prevents the chance of possibility of postoperative renal impairment following liver transplantation (10). Belghiti et al (1992) documented and developed the modified piggy-back procedure, which consisted of cavocaval anastomosis done side-to-side on the anterior aspect of the receiver’s right major hepatic vein, thereby reducing outflow obstruction (11).
Conclusion
The liver venous vasculature does show numerous variations in its draining pattern into the retro-hepatic segment of IVC. This knowledge plays a significant role in understanding the severity of hepatic venous outflow obstruction, as it depends on the number of obstructed hepatic veins (8). It is also imperative to evaluate the morphology of the venous drainage prior to any hepatic surgeries, especially in the transplantation of the liver, to prevent the massacre of life-threatening hemorrhage, thus improving postoperative outcomes.
Acknowledgement
I would like to thank my colleagues for their unending support while working on this research topic. The researchers truly acknowledge the precious souls who donated bodies to medicine to aid in research in the field of anatomy. Inferences from this study will enhance the surgeon's overall knowledge, thereby improving patient care. Therefore, the donors, with their kin, deserve our highest appreciation.
Funding sources
The authors did not receive any funding to conduct this study.
Ethical statement
The permission to conduct this study was granted by the Institutional Ethics Committee of Goa Medical College (code: GMC/IEC-20/02-01; dated 03/02/2023).
Conflicts of interest
There are no conflicts of interest between the authors.
Author contributions
- Dr Merle Casia Dias collected and analyzed the necessary data and prepared the manuscript.
- Dr Uday Kudalkar contributed to the analysis and interpretation of the data.
- Dr Nilam Madhale contributed to the analysis and interpretation of the data.
- Dr. Abhishek Krishnanath Kavlekar assisted in collecting and analyzing the necessary data, along with the preparation of the manuscript.
Article Type: Research |
Subject:
Basic medical sciences
References
1. Williams P, editor. Gray's Anatomy. 38th ed. Edinburgh: Churchill Livingstone; 1995. P.1902-3 [View at Publisher]
2. Hung Vinh Tran, Nghia Thanh Vo, Hai Van Duong, Ernest F Talarico. Anatomical variations of hepatic veins in Vietnamese adults. Eur J Anat. 2020;24(2):99-109. [View at Publisher] [Google Scholar]
3. Hollinshead HW. Anatomy for surgeons. 1st volume. 2nd ed. NewYork: Harper & Row; 1971. P.325-327. [View at Publisher]
4. Nicolas AM. Blood supply and anatomy of the upper abdominal organs. London: Pitman Medical Publishing; 1955. P.548-549. [View at Publisher]
5. Camargo AM, Texeira GG, Ortale JR. Anatomy of the ostia venae hepaticae and the retro-hepatic segment of the Inferior vena cava. J Anat. 1996;188(1):59-64. [View at Publisher]
6. Meunier B, Bardaxoglou E, Spiliopoulos G, Landen S, Camus C, Roumeas J, et al. Liver transplantation with preservation of the inferior vena cava and 'piggyback' reimplantation of the liver. Ann Chir. 1994;48(11):986-8. [View at Publisher] [PMID] [Google Scholar]
7. Fersia O, Dawson D. Evaluation Of The Variations Of The Hepatic Veins. The Internet Journal of Human Anatomy. 2010;2(1). [View at Publisher]
8. Romans G J, ed. Cunningham's textbook of anatomy. 12th ed. Oxford: University Press; 1981. p.945. [View at Publisher] [Google Scholar]
9. Fang CH, You JH, Lau WY, Lai EC, Fan YF, Zhong SZ, et al. Anatomical variations of hepatic veins: three-dimensional computed tomography scans of 200 subjects. World J Surg. 2012;36(1):120-4. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Chen Z Ju W, Chen C, Wang T, Yu J, Hong X, et al. Application of various surgical techniques in liver transplantation: a retrospective study. Ann Transl Med. 2021;9(17):1367. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Belghiti J, Panis Y, Sauvanet A, Gayet B, Fékétéet F. A new technique of side-to-side caval anastomosis during orthotopic hepatic transplantation without inferior vena caval occlusion. Surg Gynecol Obstet. 1992;175(3):270-2. [View at Publisher] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).





