Volume 8, Issue 1 (Journal of Clinical and Basic Research (JCBR) 2024)
jcbr 2024, 8(1): 1-3 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Datta R R, Awasthi A. Diagnostic pitfalls of non-secretory myeloma: The biochemical perspective. jcbr 2024; 8 (1) :1-3
URL: http://jcbr.goums.ac.ir/article-1-436-en.html
URL: http://jcbr.goums.ac.ir/article-1-436-en.html
1- SRL Diagnostics, National Reference Lab, Gurugram, India , rashmi.datta@agilus.in
2- SRL Diagnostics, National Reference Lab, Gurugram, India
2- SRL Diagnostics, National Reference Lab, Gurugram, India
Keywords: Immunoglobulin Light Chains, Multiple Myeloma, Clinical Decision-Making, Clinical Laboratory Services, Para proteins
Full-Text [PDF 399 kb]
(1368 Downloads)
| Abstract (HTML) (2955 Views)
Full-Text: (833 Views)
Introduction
Non-secretory multiple myeloma (NSMM) is a rare myeloma subtype whose diagnosis is established by demonstration of monoclonal plasma cells ≥ 10% in the bone marrow and by negative results on serum and urine electrophoresis and immunofixation studies (1,2). It was first described in 1958 by Serre and accounts for 1% to 5% of all patients with multiple myeloma (1,2).
However, this subset of the myeloma population could be easily misdiagnosed in the absence of a detailed and meticulous work-up.
We discuss a case of NSMM, the significance of comprehensive work-up, and the role of serum free light chain (FLC) assays in its diagnosis.
Case Report
A 65-year-old male's serum sample was received in the study laboratory to evaluate the complete hemogram and metabolic profile. The hemogram and routine clinical chemistry reports of the patient were deranged and suggestive of multi-organ involvement. The results of the tests are mentioned in the tables below (Table 1, showing the complete hemogram and routine biochemical test findings of the patient.)
Non-secretory multiple myeloma (NSMM) is a rare myeloma subtype whose diagnosis is established by demonstration of monoclonal plasma cells ≥ 10% in the bone marrow and by negative results on serum and urine electrophoresis and immunofixation studies (1,2). It was first described in 1958 by Serre and accounts for 1% to 5% of all patients with multiple myeloma (1,2).
However, this subset of the myeloma population could be easily misdiagnosed in the absence of a detailed and meticulous work-up.
We discuss a case of NSMM, the significance of comprehensive work-up, and the role of serum free light chain (FLC) assays in its diagnosis.
Case Report
A 65-year-old male's serum sample was received in the study laboratory to evaluate the complete hemogram and metabolic profile. The hemogram and routine clinical chemistry reports of the patient were deranged and suggestive of multi-organ involvement. The results of the tests are mentioned in the tables below (Table 1, showing the complete hemogram and routine biochemical test findings of the patient.)
|
Table 1. Complete hemogram and routine biochemical test findings of the patient
 |
In view of the deranged metabolic and hematological profile, the patient history was requested; in it, it was revealed that the patient had presented to his clinician with long-term weakness and back aches. On examination, the clinician had a suspicion of anemia, possibly due to a chronic ailment. Accordingly, the patient was advised to undergo a routine complete blood count (CBC) and biochemistry examination. Magnetic resonance imaging (MRI) of the spine was also requested.
The MRI findings, as mentioned in the patient's prescription, revealed spinal osteolytic lesions (D3, D4, and D6 vertebral lesions), along with cord compression.
As the patient had a deranged kidney function, anemia, and lytic bony lesions, a gammopathy panel was requested.
The laboratory investigations in this panel were inclusive of serum protein capillary electrophoresis, FLC assays, immunoglobulin levels (IgG, IgA, and IgM), and beta 2 microglobulin and immunofixation electrophoresis (IFE). No urine specimens were available for analysis.
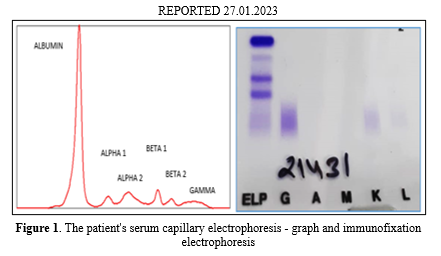
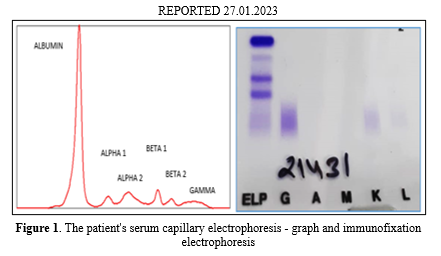
Serum capillary electrophoresis was done on the patient's serum sample in a Minicap Electrophoresis FP analyzer (Sebia Platform). Reports revealed a normal graph without any noticeable bands, distortions, or suspicious regions.
Immunofixation electrophoresis was performed on the serum sample and subsequently on HYDRASYS agarose gel electrophoresis apparatus by Sebia (Norcross, GA, USA), according to the manufacturer's instructions. Individual antisera against IgG, IgA, and IgM heavy chains and kappa and lambda light chains were applied. No monoclonal proteins were identified following staining of the immunoprecipitates (Figure 1, showing the patient's serum capillary electrophoresis-graph and IFE).
The MRI findings, as mentioned in the patient's prescription, revealed spinal osteolytic lesions (D3, D4, and D6 vertebral lesions), along with cord compression.
As the patient had a deranged kidney function, anemia, and lytic bony lesions, a gammopathy panel was requested.
The laboratory investigations in this panel were inclusive of serum protein capillary electrophoresis, FLC assays, immunoglobulin levels (IgG, IgA, and IgM), and beta 2 microglobulin and immunofixation electrophoresis (IFE). No urine specimens were available for analysis.
Serum capillary electrophoresis was done on the patient's serum sample in a Minicap Electrophoresis FP analyzer (Sebia Platform). Reports revealed a normal graph without any noticeable bands, distortions, or suspicious regions.
Immunofixation electrophoresis was performed on the serum sample and subsequently on HYDRASYS agarose gel electrophoresis apparatus by Sebia (Norcross, GA, USA), according to the manufacturer's instructions. Individual antisera against IgG, IgA, and IgM heavy chains and kappa and lambda light chains were applied. No monoclonal proteins were identified following staining of the immunoprecipitates (Figure 1, showing the patient's serum capillary electrophoresis-graph and IFE).
Duly informed patient consent was obtained before publishing the data. The identity of the patient was not revealed during the course of publishing.
Other tests were also done as a part of the gammopathy panel (Siemens BNII Nephelometer), results of which are as follows: (Table 2, showing the patient's gammopathy panel results.)
Other tests were also done as a part of the gammopathy panel (Siemens BNII Nephelometer), results of which are as follows: (Table 2, showing the patient's gammopathy panel results.)
Table 2. The patient's gammopathy panel results |
The patient history, deranged blood biochemistry and hematological results, imaging studies, and the findings of the comprehensive myeloma panel were suggestive of NSMM. However, the patient's urine sample was not available for analysis. Owing to elevated kappa FLC levels and abnormal FLC ratio, the patient may be considered to have a case of myeloma, oligo secretory type.
The patient and the clinician were further advised to conduct a bone marrow examination with immunohistochemistry (IHC) and a biopsy of the lytic lesions of the spine to reveal the presence of clonal plasma cells. However, the clinician had to refer the patient to an Oncology Institute for further management, and the patient was lost to follow-up; therefore, his further work-up was not done in the study lab.
Discussion
The classical definition of NSMM encompasses clonal bone marrow plasma cells ≥10% or biopsy-established plasmacytoma, end organ damage, and lack of serum/urinary monoclonal protein on electrophoresis and immunofixation (2,3). Nevertheless, on IHC, 85% of non-secretory myelomas stain for cytoplasmic M protein, indicative of immunoglobulin synthesis. The residual 15% is the non-producer subtype (4). The proposed pathophysiology for NSMM comprises reduced immunoglobulin synthesis, secretion defects, and rapid intracellular or extracellular immunoglobulin (Ig) degradation (5). However, the exact mechanism still remains poorly understood (6).
With the advances in detection techniques, higher sensitive methods allow the identification of monoclonal FLC in the serum/urine of the patients (4), even when usual serum and urine electrophoresis show the absence of monoclonal Ig (7). Such cases may be considered to be minimally secretory or oligo-secretory.
Oligo secretory NSMM produces predominantly or solely serum FLCs in the absence of a heavy chain (3). These patients usually do not present with classical features of multiple myeloma. Hence, their diagnosis is challenging and depends on meticulous clinical assessment and detailed patient work-up. Due to the absence of quantifiable monoclonal protein in the patient's serum/urine, these cases are often misdiagnosed. Also, due to its less serological involvement, the disease's staging and monitoring remain unclear. A high index of notion for NSMM should be taken into account when excluding multiple myeloma as the cause of pain, lytic lesions, and positive bone scans.
In the present case, end-organ involvement, as evidenced by the patient's metabolic profile and the lytic bone lesions on the MRI report, prompted the clinician to opt for gammopathy evaluation. The secretory activity of myeloma was established biochemically by the raised FLC ratio (kappa/lambda ratio = 265.890) in the absence of bone marrow biopsy and IHC report, while serum electrophoresis together with IFE did not reveal the presence of any monoclonal protein. Conclusively, the above findings were highly suggestive of NSMM, oligo secretory subtype, and the patient/clinician was further advised on bone marrow biopsy with IHC to establish a confirmatory diagnosis.
Based on the literature, kappa (κ) non-secretory myelomas have been reported to be 4 times more common than the lambda (λ) type (6). κ light chain oligo secretion was reported in our case as well.
The role of serum FLCs and the FLC ratio in the diagnosis and management of NSMM has been subdued to date.
The current definition of NSMM by the International Myeloma Working Group does not take into account the serum FLC levels and their ratio (FLC ratio), which may be revisited as the oligo secretory NSMM subtype is actively secreting an immunoglobulin component (3).
Moreover, monitoring the patient's response to therapy in NSMM is arduous because of the inability to use serum/urine immunoglobulin as a measure of tumor burden. As a consequence, monitoring NSMM relies heavily on PET/CT scans and frequent bone marrow sampling. Serial bone marrow examination for quantification of neoplastic plasma cell infiltration is considered the gold standard. However, the time consumed, cost, and the patient discomfort associated with it make it a less viable choice from a practical point of view (8).
Previous studies have recommended the use of FLC assays in establishing diagnosis of NSMM and monitoring therapies (2,4). Considering their easy quantification, cost efficacy, and minimal patient discomfort, the FLC assay and ratio qualify as a suitable adjunct to the existing techniques.
Further studies and a retrospective literature review are needed to determine conclusively the utility of pre-treatment FLC assay, serial FLC values, and FLC ratio in monitoring patient therapy. Additionally, the role of FLC assay and ratio in diagnosing, staging, and management of NSMM should also be evaluated.
Conclusion
In conclusion, the absence of paraprotein does not exclude an NSMM diagnosis. The FLC assays help diagnose the oligo-secretory subtype, which can be further validated by confirmatory diagnostic testing. Its usefulness in monitoring treatment effects and disease management needs further studies and investigation.
Acknowledgement
The authors would like to acknowledge the clinical chemistry technical staff involved in sample processing and obtaining patient history -- Mr. Rohit and Mr. Mustaque.
Funding sources
The authors did not receive support from any organization for the submitted work.
Ethical statement
Duly informed patient consent was obtained before publishing the data. The identity of the patient was not revealed during the course of publishing.
Conflicts of interest
The authors do not have any conflicts of interest.
Author contributions
1. Dr. Rashmi Rasi Datta: Study conception and design, data collection, analysis and interpretation of results, and manuscript preparation; 2. Dr. Ashutosh Awasthi: Review and approval of the final manuscript. All authors read and approved the final manuscript.
The patient and the clinician were further advised to conduct a bone marrow examination with immunohistochemistry (IHC) and a biopsy of the lytic lesions of the spine to reveal the presence of clonal plasma cells. However, the clinician had to refer the patient to an Oncology Institute for further management, and the patient was lost to follow-up; therefore, his further work-up was not done in the study lab.
Discussion
The classical definition of NSMM encompasses clonal bone marrow plasma cells ≥10% or biopsy-established plasmacytoma, end organ damage, and lack of serum/urinary monoclonal protein on electrophoresis and immunofixation (2,3). Nevertheless, on IHC, 85% of non-secretory myelomas stain for cytoplasmic M protein, indicative of immunoglobulin synthesis. The residual 15% is the non-producer subtype (4). The proposed pathophysiology for NSMM comprises reduced immunoglobulin synthesis, secretion defects, and rapid intracellular or extracellular immunoglobulin (Ig) degradation (5). However, the exact mechanism still remains poorly understood (6).
With the advances in detection techniques, higher sensitive methods allow the identification of monoclonal FLC in the serum/urine of the patients (4), even when usual serum and urine electrophoresis show the absence of monoclonal Ig (7). Such cases may be considered to be minimally secretory or oligo-secretory.
Oligo secretory NSMM produces predominantly or solely serum FLCs in the absence of a heavy chain (3). These patients usually do not present with classical features of multiple myeloma. Hence, their diagnosis is challenging and depends on meticulous clinical assessment and detailed patient work-up. Due to the absence of quantifiable monoclonal protein in the patient's serum/urine, these cases are often misdiagnosed. Also, due to its less serological involvement, the disease's staging and monitoring remain unclear. A high index of notion for NSMM should be taken into account when excluding multiple myeloma as the cause of pain, lytic lesions, and positive bone scans.
In the present case, end-organ involvement, as evidenced by the patient's metabolic profile and the lytic bone lesions on the MRI report, prompted the clinician to opt for gammopathy evaluation. The secretory activity of myeloma was established biochemically by the raised FLC ratio (kappa/lambda ratio = 265.890) in the absence of bone marrow biopsy and IHC report, while serum electrophoresis together with IFE did not reveal the presence of any monoclonal protein. Conclusively, the above findings were highly suggestive of NSMM, oligo secretory subtype, and the patient/clinician was further advised on bone marrow biopsy with IHC to establish a confirmatory diagnosis.
Based on the literature, kappa (κ) non-secretory myelomas have been reported to be 4 times more common than the lambda (λ) type (6). κ light chain oligo secretion was reported in our case as well.
The role of serum FLCs and the FLC ratio in the diagnosis and management of NSMM has been subdued to date.
The current definition of NSMM by the International Myeloma Working Group does not take into account the serum FLC levels and their ratio (FLC ratio), which may be revisited as the oligo secretory NSMM subtype is actively secreting an immunoglobulin component (3).
Moreover, monitoring the patient's response to therapy in NSMM is arduous because of the inability to use serum/urine immunoglobulin as a measure of tumor burden. As a consequence, monitoring NSMM relies heavily on PET/CT scans and frequent bone marrow sampling. Serial bone marrow examination for quantification of neoplastic plasma cell infiltration is considered the gold standard. However, the time consumed, cost, and the patient discomfort associated with it make it a less viable choice from a practical point of view (8).
Previous studies have recommended the use of FLC assays in establishing diagnosis of NSMM and monitoring therapies (2,4). Considering their easy quantification, cost efficacy, and minimal patient discomfort, the FLC assay and ratio qualify as a suitable adjunct to the existing techniques.
Further studies and a retrospective literature review are needed to determine conclusively the utility of pre-treatment FLC assay, serial FLC values, and FLC ratio in monitoring patient therapy. Additionally, the role of FLC assay and ratio in diagnosing, staging, and management of NSMM should also be evaluated.
Conclusion
In conclusion, the absence of paraprotein does not exclude an NSMM diagnosis. The FLC assays help diagnose the oligo-secretory subtype, which can be further validated by confirmatory diagnostic testing. Its usefulness in monitoring treatment effects and disease management needs further studies and investigation.
Acknowledgement
The authors would like to acknowledge the clinical chemistry technical staff involved in sample processing and obtaining patient history -- Mr. Rohit and Mr. Mustaque.
Funding sources
The authors did not receive support from any organization for the submitted work.
Ethical statement
Duly informed patient consent was obtained before publishing the data. The identity of the patient was not revealed during the course of publishing.
Conflicts of interest
The authors do not have any conflicts of interest.
Author contributions
1. Dr. Rashmi Rasi Datta: Study conception and design, data collection, analysis and interpretation of results, and manuscript preparation; 2. Dr. Ashutosh Awasthi: Review and approval of the final manuscript. All authors read and approved the final manuscript.
Article Type: Case report |
Subject:
Oncology
References
1. Blade J, Kyle RA. Nonsecretory myeloma, immunoglobulin D myeloma and plasma cell leukemia. Hematol Oncol Clin North Am. 1999;13:1259-72. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Drayson M, Tang LX, Drew R, Mead GP, Carr-Smith H, Bradwell AR. Serum free light-chain measurements for identifying and monitoring patients with nonsecretory multiple myeloma. Blood. 2001;97(9):2900-2. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Corso A., Mangiacavalli S. Non-secretory myeloma: ready for a new definition? Mediterr J Hematol Infect Dis. 2017;9(1):e2017053. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Khurana U, Joshi D, Santoshi JA, Sharma T, Kapoor N. Oligosecretory multiple myeloma: a case report. Blood Res. 2016;51(1):63-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Coriu D, Weaver K, Schell M, Eulitz M, Murphy CL, Weiss DT, et al. A molecular basis for nonsecretory myeloma. Blood. 2004;104(3):829-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Dupuis MM, Tuchman SA. Non-secretory multiple myeloma: from biology to clinical management. Onco Targets Ther. 2016;9:7583-90. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Shaw GR. Nonsecretory plasma cell myeloma-becoming even rarer with serum free light-chain assay: a brief review. Arch Pathol Lab Med. 2006;130:1212-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Kelley MA, Mestre A, Ayau MF, Arpit A, Ratesh K. A Case Report of Non-secretory Multiple Myeloma. Cureus. 2022;14(9):e29571. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






