Volume 7, Issue 4 (Journal of Clinical and Basic Research (JCBR) 2023)
jcbr 2023, 7(4): 1-4 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zakeri S, Moradi F, Kolangi F. What is a healthy lifestyle for breast cancer prevention from the perspective of Iranian and modern medicine? A systematic review. jcbr 2023; 7 (4) :1-4
URL: http://jcbr.goums.ac.ir/article-1-415-en.html
URL: http://jcbr.goums.ac.ir/article-1-415-en.html
1- Department of Persian Medicine, School of Persian Medicine, Babol University of Medical Sciences, Babol, Iran
2- Department of Persian Medicine, School of Persian Medicine, Tehran University of Medical Sciences, Tehran, Iran
3- Department of Persian Medicine, Counseling and Reproductive Health Research Centre, Golestan University of Medical Sciences, Gorgan, Iran
2- Department of Persian Medicine, School of Persian Medicine, Tehran University of Medical Sciences, Tehran, Iran
3- Department of Persian Medicine, Counseling and Reproductive Health Research Centre, Golestan University of Medical Sciences, Gorgan, Iran
Full-Text [PDF 494 kb]
(920 Downloads)
| Abstract (HTML) (1963 Views)
Full-Text: (557 Views)
Introduction
Breast cancer is the most prevalent and deadly cancer among women, which is responsible for 14% of total cancer deaths annually (1, 2). New cases and mortality of breast cancer are reported to be 52% and 62%, respectively, in developed countries (3). Since this disease has no obvious signs in the beginning, patients are generally diagnosed at advanced stages when the curative effect of treatment decreases (4). A high incidence of emotional complications such as anxiety and depression interrupt the daily life of breast cancer patients. Other disruptive problems are the side effects of chemotherapy, surgery, and radiotherapy (5). The absence of decisive therapeutic and preventive strategies for breast cancer relapse, expenditures, and the burden of the disease are the other usual concerns (6, 7). It is estimated that disability from breast cancer will increase to 26% by 2026, which causes more concern and urgent necessity for the prevention and control of this problem (8).
Complementary and alternative medicine (CAM) has been viewed positively by the general public in recent years (9). With the increase in breast cancer prevalence, attention to CAM is increasing, too (10).
Iranian medicine (IM), as a part of CAM formed on the Iranian plateau thousands of years ago (11), provides therapeutic guidelines and helpful preventive recommendations for cancers (12). Along with discovering new therapeutic ways, it seems better to recognize the predisposing factors of breast cancer to prevent its consequences. Approving many IM theories by new studies may be worthwhile to prevent breast cancer.
Methods
This review study was carried out by searching medical textbooks of IM, including the Canon of Medicine (13), Zakhireh Kharazmshahi (14), Exir-e A'zam (15), Hedayat al-Mota'allemin fi al-Tibb (16), and al-Hawi (17), with keywords related to lifestyle modification in traditional medicine, which is called Setteye Zarooriyeh, such as sufficient movement and rest, consuming proper drink and food, proper excretion and retention, good ambient air, suitable sleep and wakefulness, and psychological and mental reactions. The data were obtained from a complete review of the materials related to the definition, etiology, and general points of breast cancer risk factors. This review study was carried out for the last 21 years (2001-2022) using specific keywords related to breast cancer risk factors in PubMed, Scopus, and Science Direct and then compared to the most famous IM manuscripts. Finally, relevant findings were categorized and compared with the IM context.
Results and Discussion
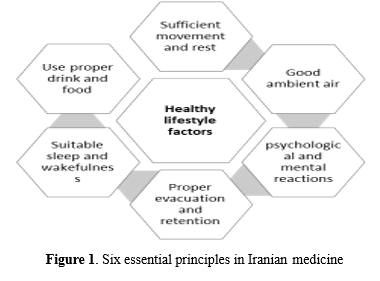
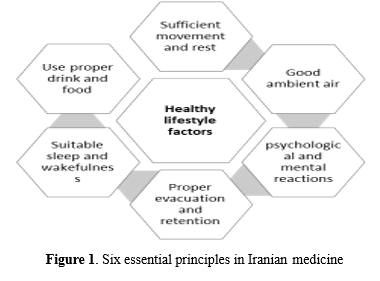
The health of organs, including the breast tissue, is a subset of the health of the body to preserve it; traditional medicine recommends lifestyle modification in 6 main areas, called Setteye Zarooriyeh.
The 6 essential principles of life, the observance of which is an important foundation of health, include sufficient movement and rest, consuming proper drink and food, proper evacuation and retention, good ambient air, suitable sleep and wakefulness, and psychological and mental reactions (13, 14) (Figure 1).
Each of these helps maintain the health of other organs by strengthening the body as a whole.
1. Sufficient movement and rest:
The current evidence confirms some IM theories about the risk factors of breast cancer. One of them is physical inactivity. Based on IM didactics, physical activity is an element of a healthy lifestyle that protects the body from the accumulation of pathogenic temperaments by strengthening excretory forces (14). Avicenna believed that physical activity removes residuals from the body in a safe way without any danger or trouble. Therefore, it is a preventive way for many diseases (13). In this regard, recent studies have confirmed that exercise has a preventive effect on cancer; although the exact mechanism is unknown, the impact on the immune system, steroid hormones or insulin/insulin-like growth factors, free radical generation, alteration in body composition or weight, and direct effects on cancer cells are the proposed mechanisms (18). Nowadays, exercise is well-known as an anti-inflammatory procedure that counteracts muscle catabolism by increasing protein synthesis and reversing protein degradation and, therefore, confronts cancer cachexia (19). Investigators have revealed that women who regularly exercise 5 hours a week had a 35% reduction in the risk of breast cancer incidence compared with those who had sedentary life (20). Retrospective studies have also demonstrated that hiking 10 hours weekly has a significant effect on breast cancer risk reduction (21). Physical activity was also associated with a reduction in the odds of breast cancer (22). Indeed, exercise decreases the complication of cardiopulmonary events in breast cancer patients (23).
2. Consuming proper drink and food:
Studies show that diet affects the incidence of breast cancer, its recurrence, and prognosis. New medical sources point to the role of a variety of foods in causing or preventing cancer. Modern medicine has not mentioned the etiquette of eating, the order and timing of it, and has referred to general dietary recommendations, including reducing alcohol, red meat, and overall fat intake, and increasing the consumption of vegetables and fruits. Consumption of fried meat is a risk factor in genetically predisposed individuals. It considers the prevention of breast cancer by using the diet to be dependent on a separate and proportionate mixed diet, rich in basic foods and traditional methods of food production and cooking (24, 25). Iranian traditional medicine refers to nutritional etiquette, avoiding mixing certain foods, and communal eating, etc., and also mentions some valuable points about drinking and eating etiquette (15, 17).
Regarding the principles of a healthy diet, IM physicians believed that beef intake increased the production of pathogenic unnatural humor, the burned black bile (26). According to the theory of humors in IM, a balanced proportion of humors can be very important. Their disproportion can qualitatively or quantitatively result in different diseases. Moreover, increasing black bile is a cause of menses retention. As a result, beef intake has a dual causative effect on breast cancer (13, 15, 17). Long-term consumption of high-fat foods increases the risk of breast cancer by raising serum estrogen levels (27). New in vitro studies have confirmed the carcinogenic role of red and processed meat via increasing the number of preneoplastic cells by heme iron, which promotes lipid peroxidation (28). Recent studies have shown that diet modification is a protective and preventive factor for breast cancer (29). A retrospective study has shown that red meat consumption in adolescence can increase the risk incidence of breast cancer during menopause (30). Another study claimed that reducing dietary fat intake with mild body weight loss may improve the relapse of breast cancer (31). Several studies show that some dietary compounds have epigenetic targets in cancer cells and may play a role in cancer prevention (32).
3. Proper evacuation and retention
Proper evacuation is necessary to expel some substances from the body and excrete them. Besides, the retention of some other substances and their confinement is necessary for the maintenance of the body's health (13, 14).
From the viewpoint of IM manuscripts, breastfeeding has benefits for both mother and infant and keeps their bodies away from much harm. Sucking breast by the infant and the secretion of milk from the mother's body has preventive effects against the accumulation of pathogenic temperaments (33). Besides, in epidemiologic studies, breastfeeding reduces the risk of breast cancer. Indeed, prolonged breastfeeding causes fewer women to be afflicted with this disease (34).
Another predisposing factor for breast cancer in IM is obesity, which is also noted as a cause of menstrual retention. Weight loss is an important step for regulating menstruation to prevent subsequent complications (17). This theory is in line with recent findings. Some researchers have pointed out that obesity can increase the risk of breast cancer, especially at menopausal ages (35). According to researchers, obesity is associated with altered adipose tissue function. Chronic low-grade inflammation, adipocyte death, immune cell infiltration, and remodeling are present in the obese body, making it prone to pathophysiologic changes and possibly promoting breast and other cancers (36).
There is a link between obesity and an increased risk of breast cancer (37). Since most estrogen in postmenopausal women is converted from androstenedione to estrogen by the adipose tissue, obesity is associated with a long-term increase in estrogen exposure. Estrogen plays an important role in the development and spread of breast cancer (38).
In IM, daily, complete, and soft defecation is regarded as a natural way to inhibit the retention of pathogenic temperaments and prevent many diseases (13, 17). In recent studies, a relationship between chronic constipation and a rise in the risk of breast cancer has been identified (39). New evidence has revealed that a high-fiber diet in early adulthood significantly reduces the risk of breast cancer (40). Constipation should be treated at any time, whether a person has constipation without cancer, or when they are diagnosed with cancer, or when they are undergoing cancer treatment (41).
Recent studies have hypothesized about the effect of intestinal and breast microbiome on breast cancer; changes in the composition and function of several bacterial species of breast and intestine may lead to the development of breast cancer through several pathways. One of the most prominent roles of the gut microbiota is to regulate the metabolism of steroid hormones such as estrogens, an element that plays a key role in the growth of breast cancer, especially in postmenopausal women (42). Prolonged fecal stasis in the large intestine of patients with constipation affects the microbial environment of the large intestine (43).
From the perspective of IM, one way to excrete waste from the body is menstruation. Ahmad Akhawayni Bukhari (?–983 AD), one of the oldest IM physicians in the Middle Ages, has several discussions and theories about cancer and its reasons in his famous book "Hidayat al-Mutaallimin fi al-Tibb" (The Students' Handbook of Medicine). He believed that the reason for cancer is the body's failure to purge pathogenic temperaments. He also mentioned that "melancholic swelling" is a subsequence of menses retention, which can lead to breast cancer in women with delayed menstruation (16). Avicenna believed that timely and enough menstruation rescues women's bodies from excess pathogenic temperaments and is a sign of complete well-being. In contrast, retention of the menses (amenorrhea or oligomenorrhea) during childbearing ages leads to the accumulation of pathogenic temperaments and subsequent complications (13) (Table 1).
One complication of menses retention in IM is tissue swelling, which involves an organ by altering the shape, size, and function of the related organs (13) (Figure 2).

The prisoners of IM believed that pathogenic temperaments could shift from the uterus to the breast via the intravenous contribution between them, so the diseases and dysfunctions of the uterus and breast can affect each other. They mentioned that the mechanism of menses retention during pregnancy is an exception. The menses blood transforms into the fetus's nutrition during pregnancy, and after labor, it changes to milk for breastfeeding (13, 17). The amount of menses blood affects the quality of milk, and regular menstruation is the only definite cure for some breast diseases (17).
There are new relevant studies about the role of menses retention as a predisposing factor for breast cancer. Increased exposure to estrogen is associated with an increased risk of breast cancer. Moderate exercise, breastfeeding, and factors that have a protective effect. The final differentiation of the breast cell associated with the completion of the gestation period also has a protective effect.
4. Good ambient air and environment
From the perspective of IM, the quality of the ambient air has a direct effect on the temperaments of the body and soul. Inhaled air will enter the lungs, blood circulation, and cells; as a result, it will have an undeniable impact on the process of metabolism and cellular respiration (14). Avicenna believes that inhaled air should not be mixed with inappropriate substances (13). Environmental toxins can have adverse health impacts through changes in epigenetic regulation. Exposure to polycyclic aromatic hydrocarbons, nitrogen dioxide, and gaseous contaminants alters the methylation of tumorigenic genes in the breast (44, 45). Many chemicals with estrogenic activity in the environment can enter the human breast. A range of toxins and polychloride biphenyl with estrogen-like properties have been measured in human breast adipose tissue and human milk. These chemicals enter the environment through various means, such as food and climate, and due to their fat-loving properties, they reach the breast and accumulate in the breast fat (46). Other studies have also shown that aluminum is a metalloestrogen and can develop cancer in breast cells; in particular, it can cause genomic instability and improper proliferation in breast epithelial cells (47).
5. Psychological and mental reactions
In IM, the set of changes in human moods is called "Aeraze nafsani". Its effect on the body and health is much faster than the effect of food and drinks. If people are chronically affected by psychological emotions, the effects of various diseases will manifest (13, 14). Psychological factors such as stress, anxiety, and depression can predict the risk of breast cancer. A proposed biological mechanism for the risk of stress-related cancer includes neuroendocrine changes in the hypothalamic-adrenal-pituitary axis, which regulates the release of glucocorticoids, cortisol, catecholamine levels, and reactive species that damage the deoxyribonucleic acid (DNA) (48).
Emotional problems can be a factor in suppressing the immune system. The role of depression, loss, sadness, and anxiety in the etiology of breast cancer has been described in the 19th century. Women who suffer from depression and anxiety are more likely to develop cancer.
Observations of the presence of a personality type prone to cancer and the existence of an association between emotional states and breast cancer have been reported by other physicians. Susceptibility to the disease appears to be related to women who have a hysterical, melancholic, depressed, and are unable to vent their anger (48).
The findings of the systematic review study indicate that psychological factors may play an important role in the etiology of cancers such as breast and lung cancers. They can influence cancer development (49).
For the prevention and control of breast cancer in women, the findings suggest that doctors and nurses should emphasize psychological factors in women's health education.
6. Sleep: Suitable sleep and wakefulness
The IM manuscripts declare that having regular and enough sleep helps the body forces to digest and repeal pathogenic temperaments (13, 16).
New studies have confirmed that having a regular sleep rhythm leads to the regular release of melatonin with anti-estrogenic effects, so it reduces the risk of hormone-dependent breast cancer (50). Plasma melatonin binds to proteins such as albumin and alpha-glycoprotein and enters all cells in tissues. Melatonin stimulates the immune system and increases interleukin products, which are involved in the regulation of immune responses. Extensive functions of melatonin in breast cancer include induction of apoptosis, telomerase inhibition, epidermal growth factors in cancer cells, cell cycle inhibition, antioxidant role, and free radicals. melatonin stimulates the immune system to destroy cancer cells, repair damaged DNA, regulate daily and seasonal rhythms, and inhibit angiogenesis (51). Some studies have revealed that breast cancer is more common among women who work night shifts (52). Light at night may also increase the risk of breast cancer by inhibiting nocturnal melatonin secretion, which leads to high levels of estrogen circulation (51).
Sleep quality characteristics are associated with inflammatory markers in women's breast tissue (53). Sleep patterns are also linked to cancer. A longer sleep duration may significantly increase the risk of breast cancer, especially estrogen-positive breast cancer (54).
Conclusion
The results of comparing the healthy lifestyle in preventing breast cancer from the perspective of Iranian and modern medicine and new studies were the same. Increased exposure to estrogen is associated with a higher risk of breast cancer. Considering the importance of disease prevention from the perspective of IM, it seems that providing the proper lifestyle and introducing the 6 essential principles (sufficient movement and rest, consuming appropriate drink and food, proper evacuation and retention, good ambient air, suitable sleep and wakefulness, and psychological and mental reactions) for maintaining health from the perspective of this medical school can play an essential role in preventing breast diseases.
Acknowledgement
Not applicable.
Funding sources
This article does not have any financial support.
Ethical statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author contributions
All the authors contributed to editing the manuscript comprehensively and confirmed the final version of the paper.
Breast cancer is the most prevalent and deadly cancer among women, which is responsible for 14% of total cancer deaths annually (1, 2). New cases and mortality of breast cancer are reported to be 52% and 62%, respectively, in developed countries (3). Since this disease has no obvious signs in the beginning, patients are generally diagnosed at advanced stages when the curative effect of treatment decreases (4). A high incidence of emotional complications such as anxiety and depression interrupt the daily life of breast cancer patients. Other disruptive problems are the side effects of chemotherapy, surgery, and radiotherapy (5). The absence of decisive therapeutic and preventive strategies for breast cancer relapse, expenditures, and the burden of the disease are the other usual concerns (6, 7). It is estimated that disability from breast cancer will increase to 26% by 2026, which causes more concern and urgent necessity for the prevention and control of this problem (8).
Complementary and alternative medicine (CAM) has been viewed positively by the general public in recent years (9). With the increase in breast cancer prevalence, attention to CAM is increasing, too (10).
Iranian medicine (IM), as a part of CAM formed on the Iranian plateau thousands of years ago (11), provides therapeutic guidelines and helpful preventive recommendations for cancers (12). Along with discovering new therapeutic ways, it seems better to recognize the predisposing factors of breast cancer to prevent its consequences. Approving many IM theories by new studies may be worthwhile to prevent breast cancer.
Methods
This review study was carried out by searching medical textbooks of IM, including the Canon of Medicine (13), Zakhireh Kharazmshahi (14), Exir-e A'zam (15), Hedayat al-Mota'allemin fi al-Tibb (16), and al-Hawi (17), with keywords related to lifestyle modification in traditional medicine, which is called Setteye Zarooriyeh, such as sufficient movement and rest, consuming proper drink and food, proper excretion and retention, good ambient air, suitable sleep and wakefulness, and psychological and mental reactions. The data were obtained from a complete review of the materials related to the definition, etiology, and general points of breast cancer risk factors. This review study was carried out for the last 21 years (2001-2022) using specific keywords related to breast cancer risk factors in PubMed, Scopus, and Science Direct and then compared to the most famous IM manuscripts. Finally, relevant findings were categorized and compared with the IM context.
Results and Discussion
The health of organs, including the breast tissue, is a subset of the health of the body to preserve it; traditional medicine recommends lifestyle modification in 6 main areas, called Setteye Zarooriyeh.
The 6 essential principles of life, the observance of which is an important foundation of health, include sufficient movement and rest, consuming proper drink and food, proper evacuation and retention, good ambient air, suitable sleep and wakefulness, and psychological and mental reactions (13, 14) (Figure 1).
Each of these helps maintain the health of other organs by strengthening the body as a whole.
1. Sufficient movement and rest:
The current evidence confirms some IM theories about the risk factors of breast cancer. One of them is physical inactivity. Based on IM didactics, physical activity is an element of a healthy lifestyle that protects the body from the accumulation of pathogenic temperaments by strengthening excretory forces (14). Avicenna believed that physical activity removes residuals from the body in a safe way without any danger or trouble. Therefore, it is a preventive way for many diseases (13). In this regard, recent studies have confirmed that exercise has a preventive effect on cancer; although the exact mechanism is unknown, the impact on the immune system, steroid hormones or insulin/insulin-like growth factors, free radical generation, alteration in body composition or weight, and direct effects on cancer cells are the proposed mechanisms (18). Nowadays, exercise is well-known as an anti-inflammatory procedure that counteracts muscle catabolism by increasing protein synthesis and reversing protein degradation and, therefore, confronts cancer cachexia (19). Investigators have revealed that women who regularly exercise 5 hours a week had a 35% reduction in the risk of breast cancer incidence compared with those who had sedentary life (20). Retrospective studies have also demonstrated that hiking 10 hours weekly has a significant effect on breast cancer risk reduction (21). Physical activity was also associated with a reduction in the odds of breast cancer (22). Indeed, exercise decreases the complication of cardiopulmonary events in breast cancer patients (23).
2. Consuming proper drink and food:
Studies show that diet affects the incidence of breast cancer, its recurrence, and prognosis. New medical sources point to the role of a variety of foods in causing or preventing cancer. Modern medicine has not mentioned the etiquette of eating, the order and timing of it, and has referred to general dietary recommendations, including reducing alcohol, red meat, and overall fat intake, and increasing the consumption of vegetables and fruits. Consumption of fried meat is a risk factor in genetically predisposed individuals. It considers the prevention of breast cancer by using the diet to be dependent on a separate and proportionate mixed diet, rich in basic foods and traditional methods of food production and cooking (24, 25). Iranian traditional medicine refers to nutritional etiquette, avoiding mixing certain foods, and communal eating, etc., and also mentions some valuable points about drinking and eating etiquette (15, 17).
Regarding the principles of a healthy diet, IM physicians believed that beef intake increased the production of pathogenic unnatural humor, the burned black bile (26). According to the theory of humors in IM, a balanced proportion of humors can be very important. Their disproportion can qualitatively or quantitatively result in different diseases. Moreover, increasing black bile is a cause of menses retention. As a result, beef intake has a dual causative effect on breast cancer (13, 15, 17). Long-term consumption of high-fat foods increases the risk of breast cancer by raising serum estrogen levels (27). New in vitro studies have confirmed the carcinogenic role of red and processed meat via increasing the number of preneoplastic cells by heme iron, which promotes lipid peroxidation (28). Recent studies have shown that diet modification is a protective and preventive factor for breast cancer (29). A retrospective study has shown that red meat consumption in adolescence can increase the risk incidence of breast cancer during menopause (30). Another study claimed that reducing dietary fat intake with mild body weight loss may improve the relapse of breast cancer (31). Several studies show that some dietary compounds have epigenetic targets in cancer cells and may play a role in cancer prevention (32).
3. Proper evacuation and retention
Proper evacuation is necessary to expel some substances from the body and excrete them. Besides, the retention of some other substances and their confinement is necessary for the maintenance of the body's health (13, 14).
From the viewpoint of IM manuscripts, breastfeeding has benefits for both mother and infant and keeps their bodies away from much harm. Sucking breast by the infant and the secretion of milk from the mother's body has preventive effects against the accumulation of pathogenic temperaments (33). Besides, in epidemiologic studies, breastfeeding reduces the risk of breast cancer. Indeed, prolonged breastfeeding causes fewer women to be afflicted with this disease (34).
Another predisposing factor for breast cancer in IM is obesity, which is also noted as a cause of menstrual retention. Weight loss is an important step for regulating menstruation to prevent subsequent complications (17). This theory is in line with recent findings. Some researchers have pointed out that obesity can increase the risk of breast cancer, especially at menopausal ages (35). According to researchers, obesity is associated with altered adipose tissue function. Chronic low-grade inflammation, adipocyte death, immune cell infiltration, and remodeling are present in the obese body, making it prone to pathophysiologic changes and possibly promoting breast and other cancers (36).
There is a link between obesity and an increased risk of breast cancer (37). Since most estrogen in postmenopausal women is converted from androstenedione to estrogen by the adipose tissue, obesity is associated with a long-term increase in estrogen exposure. Estrogen plays an important role in the development and spread of breast cancer (38).
In IM, daily, complete, and soft defecation is regarded as a natural way to inhibit the retention of pathogenic temperaments and prevent many diseases (13, 17). In recent studies, a relationship between chronic constipation and a rise in the risk of breast cancer has been identified (39). New evidence has revealed that a high-fiber diet in early adulthood significantly reduces the risk of breast cancer (40). Constipation should be treated at any time, whether a person has constipation without cancer, or when they are diagnosed with cancer, or when they are undergoing cancer treatment (41).
Recent studies have hypothesized about the effect of intestinal and breast microbiome on breast cancer; changes in the composition and function of several bacterial species of breast and intestine may lead to the development of breast cancer through several pathways. One of the most prominent roles of the gut microbiota is to regulate the metabolism of steroid hormones such as estrogens, an element that plays a key role in the growth of breast cancer, especially in postmenopausal women (42). Prolonged fecal stasis in the large intestine of patients with constipation affects the microbial environment of the large intestine (43).
From the perspective of IM, one way to excrete waste from the body is menstruation. Ahmad Akhawayni Bukhari (?–983 AD), one of the oldest IM physicians in the Middle Ages, has several discussions and theories about cancer and its reasons in his famous book "Hidayat al-Mutaallimin fi al-Tibb" (The Students' Handbook of Medicine). He believed that the reason for cancer is the body's failure to purge pathogenic temperaments. He also mentioned that "melancholic swelling" is a subsequence of menses retention, which can lead to breast cancer in women with delayed menstruation (16). Avicenna believed that timely and enough menstruation rescues women's bodies from excess pathogenic temperaments and is a sign of complete well-being. In contrast, retention of the menses (amenorrhea or oligomenorrhea) during childbearing ages leads to the accumulation of pathogenic temperaments and subsequent complications (13) (Table 1).

The prisoners of IM believed that pathogenic temperaments could shift from the uterus to the breast via the intravenous contribution between them, so the diseases and dysfunctions of the uterus and breast can affect each other. They mentioned that the mechanism of menses retention during pregnancy is an exception. The menses blood transforms into the fetus's nutrition during pregnancy, and after labor, it changes to milk for breastfeeding (13, 17). The amount of menses blood affects the quality of milk, and regular menstruation is the only definite cure for some breast diseases (17).
There are new relevant studies about the role of menses retention as a predisposing factor for breast cancer. Increased exposure to estrogen is associated with an increased risk of breast cancer. Moderate exercise, breastfeeding, and factors that have a protective effect. The final differentiation of the breast cell associated with the completion of the gestation period also has a protective effect.
4. Good ambient air and environment
From the perspective of IM, the quality of the ambient air has a direct effect on the temperaments of the body and soul. Inhaled air will enter the lungs, blood circulation, and cells; as a result, it will have an undeniable impact on the process of metabolism and cellular respiration (14). Avicenna believes that inhaled air should not be mixed with inappropriate substances (13). Environmental toxins can have adverse health impacts through changes in epigenetic regulation. Exposure to polycyclic aromatic hydrocarbons, nitrogen dioxide, and gaseous contaminants alters the methylation of tumorigenic genes in the breast (44, 45). Many chemicals with estrogenic activity in the environment can enter the human breast. A range of toxins and polychloride biphenyl with estrogen-like properties have been measured in human breast adipose tissue and human milk. These chemicals enter the environment through various means, such as food and climate, and due to their fat-loving properties, they reach the breast and accumulate in the breast fat (46). Other studies have also shown that aluminum is a metalloestrogen and can develop cancer in breast cells; in particular, it can cause genomic instability and improper proliferation in breast epithelial cells (47).
5. Psychological and mental reactions
In IM, the set of changes in human moods is called "Aeraze nafsani". Its effect on the body and health is much faster than the effect of food and drinks. If people are chronically affected by psychological emotions, the effects of various diseases will manifest (13, 14). Psychological factors such as stress, anxiety, and depression can predict the risk of breast cancer. A proposed biological mechanism for the risk of stress-related cancer includes neuroendocrine changes in the hypothalamic-adrenal-pituitary axis, which regulates the release of glucocorticoids, cortisol, catecholamine levels, and reactive species that damage the deoxyribonucleic acid (DNA) (48).
Emotional problems can be a factor in suppressing the immune system. The role of depression, loss, sadness, and anxiety in the etiology of breast cancer has been described in the 19th century. Women who suffer from depression and anxiety are more likely to develop cancer.
Observations of the presence of a personality type prone to cancer and the existence of an association between emotional states and breast cancer have been reported by other physicians. Susceptibility to the disease appears to be related to women who have a hysterical, melancholic, depressed, and are unable to vent their anger (48).
The findings of the systematic review study indicate that psychological factors may play an important role in the etiology of cancers such as breast and lung cancers. They can influence cancer development (49).
For the prevention and control of breast cancer in women, the findings suggest that doctors and nurses should emphasize psychological factors in women's health education.
6. Sleep: Suitable sleep and wakefulness
The IM manuscripts declare that having regular and enough sleep helps the body forces to digest and repeal pathogenic temperaments (13, 16).
New studies have confirmed that having a regular sleep rhythm leads to the regular release of melatonin with anti-estrogenic effects, so it reduces the risk of hormone-dependent breast cancer (50). Plasma melatonin binds to proteins such as albumin and alpha-glycoprotein and enters all cells in tissues. Melatonin stimulates the immune system and increases interleukin products, which are involved in the regulation of immune responses. Extensive functions of melatonin in breast cancer include induction of apoptosis, telomerase inhibition, epidermal growth factors in cancer cells, cell cycle inhibition, antioxidant role, and free radicals. melatonin stimulates the immune system to destroy cancer cells, repair damaged DNA, regulate daily and seasonal rhythms, and inhibit angiogenesis (51). Some studies have revealed that breast cancer is more common among women who work night shifts (52). Light at night may also increase the risk of breast cancer by inhibiting nocturnal melatonin secretion, which leads to high levels of estrogen circulation (51).
Sleep quality characteristics are associated with inflammatory markers in women's breast tissue (53). Sleep patterns are also linked to cancer. A longer sleep duration may significantly increase the risk of breast cancer, especially estrogen-positive breast cancer (54).
Conclusion
The results of comparing the healthy lifestyle in preventing breast cancer from the perspective of Iranian and modern medicine and new studies were the same. Increased exposure to estrogen is associated with a higher risk of breast cancer. Considering the importance of disease prevention from the perspective of IM, it seems that providing the proper lifestyle and introducing the 6 essential principles (sufficient movement and rest, consuming appropriate drink and food, proper evacuation and retention, good ambient air, suitable sleep and wakefulness, and psychological and mental reactions) for maintaining health from the perspective of this medical school can play an essential role in preventing breast diseases.
Acknowledgement
Not applicable.
Funding sources
This article does not have any financial support.
Ethical statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author contributions
All the authors contributed to editing the manuscript comprehensively and confirmed the final version of the paper.
References
1. Hashemi M, Sanaei S, Rezaei M, Bahari G, Hashemi S, Mashhadi MA, et al. miR-608 rs4919510 C> G polymorphism decreased the risk of breast cancer in an Iranian subpopulation. Exp Oncol. 2016;38(1):57-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Sadoughi F, Afshar HL, Olfatbakhsh A, Mehrdad N. Application of canonical correlation analysis for detecting risk factors leading to recurrence of breast cancer. Iran Red Crescent Med J. 2016;18(3):e23131. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Ghoncheh M, Pournamdar Z, Salehiniya H. Incidence and mortality and epidemiology of breast cancer in the world. Asian Pac J Cancer Prev. 2016;17(S3):43-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Leal F, Liutti VT, dos Santos VCA, de Figueiredo MAN, Macedo LT, Junior JAR, et al. Neoadjuvant endocrine therapy for resectable breast cancer: a systematic review and meta-analysis. Breast. 2015;24(4):406-12. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Ozkan M. Psychosocial adaptation during and after breast cancer. Breast Disease: Springer; 2016. p. 821-52. [View at Publisher] [DOI] [Google Scholar]
6. Omam SH, Davoodi J, Asgaraabadi MH, Richard F. Comparison of the expected outcome of the mastectomy with perceived treatment outcomes based on self-efficacy in women with breast cancer. Europ Psychiatry. 2016;33:S336. [View at Publisher] [DOI] [Google Scholar]
7. El Hasasna H, Athamneh K, Al Samri H, Karuvantevida N, Al Dhaheri Y, Hisaindee S, et al. Rhus coriaria induces senescence and autophagic cell death in breast cancer cells through a mechanism involving p38 and ERK1/2 activation. Sci Rep. 2015;5:13013. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Kunnavil R, Thirthahalli C, Nooyi SC, Somanna SN, Murthy NS. Estimation of burden of female breast cancer in India for the year 2016, 2021 and 2026 using disability adjusted life years. Int J Community Med Public Health. 2016;3(5):1135-40. [View at Publisher] [DOI] [Google Scholar]
9. Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: a systematic review. Ochsner J. 2012;12(1):45-56. [View at Publisher] [PMID] [Google Scholar]
10. Vardy JL, Chan RJ, Koczwara B, Lisy K, Cohn RJ, Joske D, et al. Clinical Oncology Society of Australia position statement on cancer survivorship care. Aust J Gen pract. 2019;48(12):833-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Zakeri S, Gorji N, Akhtari M, Moeini R. Splenectomy may have more complications than currently proven. Med Hypotheses. 2018;112:43-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Zeinalian M, Eshaghi M, Sharbafchi MR, Naji H, Marandi SMM, Asgary S. A comparative study on cancer prevention principles between Iranian traditional medicine and classic medicine. Int J Prev Med. 2016;7:61. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Avicenna H. Al-Qanoon fi al-Tibb (The Canon of Medicine). Dare Ehia Attorath Al Arabi. Beirut. 2005. [View at Publisher] [Google Scholar]
14. Jorjani E. Zakhire Kharazmshahi [The Treasure of King Khwarazm]. Ehyaye Teb Institute. Qom 2011. [View at Publisher] [Google Scholar]
15. Cashti M. Exir-e-Azam [Great Elixir]. Research Institute for Islamic and Complementary Medicine. Tehran. 2008. [Google Scholar]
16. Hedayat al-mota'allemin AA. fi al-tibb (An educational guide for medical students). Mashhad: Ferdowsi University of Mashhad Publication 1992. [View at Publisher] [Google Scholar]
17. Rhazes M. Al-Hawi (Liber Continent) (in Arabic). 1st ed. Iran: Pharmaceutical Company Press. Tehran 1990.
18. Westerlind KC. Physical activity and cancer prevention-mechanisms. Med Sci Sports Exerc. 2003;35(11):1834-40. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Gould DW, Lahart I, Carmichael AR, Koutedakis Y, Metsios GS. Cancer cachexia prevention via physical exercise: molecular mechanisms. J Cachexia Sarcopenia Muscle. 2013;4(2):111-24. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Tehard B, Friedenreich CM, Oppert J-M, Clavel-Chapelon F. Effect of physical activity on women at increased risk of breast cancer: results from the E3N cohort study. Cancer Epidemiol Biomarkers Prev. 2006;15(1):57-64. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Howard RA, Leitzmann MF, Linet MS, Freedman DM. Physical activity and breast cancer risk among pre-and postmenopausal women in the US Radiologic Technologists cohort. Cancer Causes Control. 2009;20(3):323-33. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Gomes MLB, Pinto SS, Domingues MR. Physical Activity and Breast Cancer: A Case-Control Study in Southern Brazil. Nutr Cancer. 2022;74(1):149-57. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Aweto HA, Akinbo SRA, Olawale OA. Effects of combined aerobic and stretching exercises on the cardiopulmonary parameters of premenopausal and postmenopausal breast cancer survivors. Nig Q J Hosp Med. 2015;25(3):177-83. [View at Publisher] [PMID] [Google Scholar]
24. Hanf V, Gonder U. Nutrition and primary prevention of breast cancer: foods, nutrients and breast cancer risk. Eur J Obstet Gynecol Reprod Biol. 2005;123(2):139-49. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Jevtic M, Velicki R, Popovic M, Cemerlic-Adjic N, Babovic S, Velicki L. Dietary influence on breast cancer. J BUON 2010;15(3):455-61. [View at Publisher] [PMID] [Google Scholar]
26. Naghibi F, Khalaj A, Hamzeloo MM. Cancer terminologies used in the medieval texts to the early modern Iranian traditional medicine (ITM). Journal of Research on History of Medicine. 2014;3(2):63-72. [View at Publisher] [Google Scholar]
27. Principles of Schwartz Surgery. 2015. Translated by Dr. Hadi Ahmadi Amoli. Tehran Publishing. Artin Medicine. The first of autumn. 1393. Anderson, Dinaki. Branicardi, F.Charles.
28. Bastide NM, Chenni F, Audebert M, Santarelli RL, Taché S, Naud N, et al. A Central Role for Heme Iron in Colon Carcinogenesis Associated with Red Meat IntakeHeme, Unsaturated Aldehydes, and Colon Cancer. Cancer Res. 2015;75(5):870-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Mahoney MC, Bevers T, Linos E, Willett WC. Opportunities and strategies for breast cancer prevention through risk reduction. CA Cancer J Clin. 2008;58(6):347-71. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Linos E, Willett WC, Cho E, Colditz G, Frazier LA. Red meat consumption during adolescence among premenopausal women and risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2008;17(8):2146-51. [View at Publisher] [DOI] [PMID] [Google Scholar]
31. Chlebowski RT, Blackburn GL, Thomson CA, Nixon DW, Shapiro A, Hoy MK, et al. Dietary fat reduction and breast cancer outcome: interim efficacy results from the Women's Intervention Nutrition Study. J Natl Cancer Inst. 2006;98(24):1767-76. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Hardy TM, Tollefsbol TO. Epigenetic diet: impact on the epigenome and cancer. Epigenomics 2011;3(4):503-18. [View at Publisher] [DOI] [PMID] [Google Scholar]
33. Baldi A. Tadbir al-hobali va al-atfal va al-sebyan va hefz e al-sehata hom. Baghdad: dar al rashid. 1980;94. [Google Scholar]
34. Cancer CGoHFiB. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50 302 women with breast cancer and 96 973 women without the disease. Lancet. 2002;360(9328):187-95. [View at Publisher] [DOI] [PMID] [Google Scholar]
35. Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE. Adult weight change and risk of postmenopausal breast cancer. JAMA. 2006;296(2):193-201. [View at Publisher] [DOI] [PMID] [Google Scholar]
36. Iyengar NM, Gucalp A, Dannenberg AJ, Hudis CA. Obesity and cancer mechanisms: tumor microenvironment and inflammation. J Clin Oncol. 2016;34(35):4270-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
37. Naaman SC, Shen S, Zeytinoglu M, Iyengar NM. Obesity and breast cancer risk: the oncogenic implications of metabolic dysregulation. J Clin Endocrinol Metab. 2022;107(8):2154-66. [View at Publisher] [DOI] [PMID] [Google Scholar]
38. Khan MZI, Uzair M, Nazli A, Chen J-Z. An overview on Estrogen receptors signaling and its ligands in breast cancer. Eur J Med Chem. 2022;241:114658. [View at Publisher] [DOI] [PMID] [Google Scholar]
39. Sugimura T, Wakabayashi K, Nakagama H, Nagao M. Heterocyclic amines: Mutagens/carcinogens produced during cooking of meat and fish. Cancer Sci. 2004;95(4):290-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
40. Farvid MS, Eliassen AH, Cho E, Liao X, Chen WY, Willett WC. Dietary fiber intake in young adults and breast cancer risk. Pediatrics. 2016;137(3):e20151226. [View at Publisher] [DOI] [PMID] [Google Scholar]
41. Gervais C, Ducrotté P, Piche T, Di Palma M, Jovenin N, Scotté F. Constipation and cancer: Current strategies. Bull Cancer. 2016;103(9):794-804. [View at Publisher] [DOI] [PMID] [Google Scholar]
42. Laborda-Illanes A, Sanchez-Alcoholado L, Dominguez-Recio ME, Jimenez-Rodriguez B, Lavado R, Comino-Méndez I, et al. Breast and gut microbiota action mechanisms in breast cancer pathogenesis and treatment. Cancers (Basel). 2020;12(9):2465. [View at Publisher] [DOI] [PMID] [Google Scholar]
43. Zhu L, Liu W, Alkhouri R, Baker RD, Bard JE, Quigley EM, et al. Structural changes in the gut microbiome of constipated patients. Physiol Genomics. 2014;46(18):679-86. [View at Publisher] [DOI] [PMID] [Google Scholar]
44. Sahay D, Terry MB, Miller R. Is breast cancer a result of epigenetic responses to traffic-related air pollution? A review of the latest evidence. Epigenomics. 2019;11(6):701-14. [View at Publisher] [DOI] [PMID] [Google Scholar]
45. Rodgers KM, Udesky JO, Rudel RA, Brody JG. Environmental chemicals and breast cancer: an updated review of epidemiological literature informed by biological mechanisms. Environ Res. 2018;160:152-82. [View at Publisher] [DOI] [PMID] [Google Scholar]
46. Darbre PD. Environmental oestrogens, cosmetics and breast cancer. Best Pract Res Clin Endocrinol Metab. 2006;20(1):121-43. [View at Publisher] [DOI] [PMID] [Google Scholar]
47. Chappard D. Effects of aluminum on cells and tissues. Morphologie. 2016;100(329):49-50. [View at Publisher] [DOI] [PMID] [Google Scholar]
48. Paula NCNMd, Martins JAM, Amaral LM, Rhana P, Tavares EC, Leite WS, et al. Breast cancer: Is grief a risk factor? Rev Assoc Med Bras (1992). 2018;64(7):595-600. [View at Publisher] [DOI] [PMID] [Google Scholar]
49. Pereira MA, Araújo A, Simões M, Costa C. Influence of Psychological Factors in Breast and Lung Cancer Risk-A Systematic Review. Front Psychol. 2022;12:769394. [View at Publisher] [DOI] [PMID] [Google Scholar]
50. Sánchez‐Barceló EJ, Cos S, Mediavilla D, Martínez‐Campa C, González A, Alonso‐González C. Melatonin-estrogen interactions in breast cancer. J Pineal Res. 2005;38(4):217-22. [View at Publisher] [DOI] [PMID] [Google Scholar]
51. Leonardi GC, Rapisarda V, Marconi A, Scalisi A, Catalano F, Proietti L, et al. Correlation of the risk of breast cancer and disruption of the circadian rhythm. Oncol Rep. 2012;28(2):418-28. [View at Publisher] [DOI] [PMID] [Google Scholar]
52. Knutsson A. Health disorders of shift workers. Occup Med. 2003;53(2):103-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
53. Chang S-L, Durocher F, Diorio C. Sleep quality traits correlate with inflammatory markers in the breast tissue of women. Cytokine 2022;160:156028. [View at Publisher] [DOI] [PMID] [Google Scholar]
54. Lu C, Sun H, Huang J, Yin S, Hou W, Zhang J, et al. Long-term sleep duration as a risk factor for breast cancer: evidence from a systematic review and dose-response meta-analysis. Biomed Res Int. 2017;2017:4845059. [View at Publisher] [DOI] [PMID] [Google Scholar]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).